Text by Henrylito D. Tacio
Photos: testicularawarenessfoundation.com, familydoctor.org, Mayo Clinic
Prostate cancer may be the most known type of cancer among men when it comes to reproductive health. But what most men don’t know is that several types of cancer develop in the testicles.
If the type of cancer is discovered early, the man can still live longer. When former professional road racing cyclist Lance Armstrong found out that his Stage 4 testicular cancer had already spread to his lungs and brain, he underwent immediate surgery and chemotherapy. He recovered soon.
But there were so many who were not lucky. Among those who died of testicular cancer include English actor Peter William Postlethwaite, English journalist and broadcaster Frederick Richard Dimbleby, Swedish racing driver Gunnar Nilsson, US professional football player Louis Brian Piccolo, American football center Daniel Anthony Turk, Argentine soccer goalkeeper Gustavo Danie Eberto, American singer-songwriter Josh Clayton-Felt, Hungarian military officer and politician Gyula Gombos de Jakfa, and Canadian hockey player and coach James Arthur Christopher Koleff.
The testicles (also called the testes; a single testicle is called a testis) are part of the male reproductive system. These two organs are each normally somewhat smaller than a golf ball in adult males and are contained within a sac of skin called the scrotum. The scrotum hangs beneath the base of the penis; usually, the left testis hangs slightly lower than the right one.
According to The Merck Manual of Medical Information, the testes have two functions: producing sperm (the male cells needed to fertilize a female egg cell to start a pregnancy) and testosterone (the primary male sex hormone).
Types of testicular cancer
“Most testicular cancers develop in men younger than age 40,” the Merck manual points out. The testicles, however, are made up of several types of cells, each of which can develop into one or more types of cancer. Among the types of cancer that develop in the testes are non-seminoma, seminoma, teratoma, embryonal carcinoma, and choriocarcinoma.
The www.cancer.org gives the following information about these types of cancer:
Seminoma and non-seminoma cells look very different under a microscope. These two types occur about equally. Many testicular cancers contain both seminoma and non-seminoma cells. These mixed germ cell tumors are treated as non-seminomas because they grow and spread like non-seminomas.
Teratomas are germ cell tumors with areas that, under a microscope, look like each of the three layers of a developing embryo: the endoderm (innermost layer), mesoderm (middle layer), and ectoderm (outer layer).
Embryonal carcinoma is a type of non-seminoma; it is present to some degree in about 40% of testicular tumors, but pure embryonal carcinomas occur only 3-4% of the time. When seen under a microscope, these tumors can look like tissues of very early embryos.
Testicular self exam 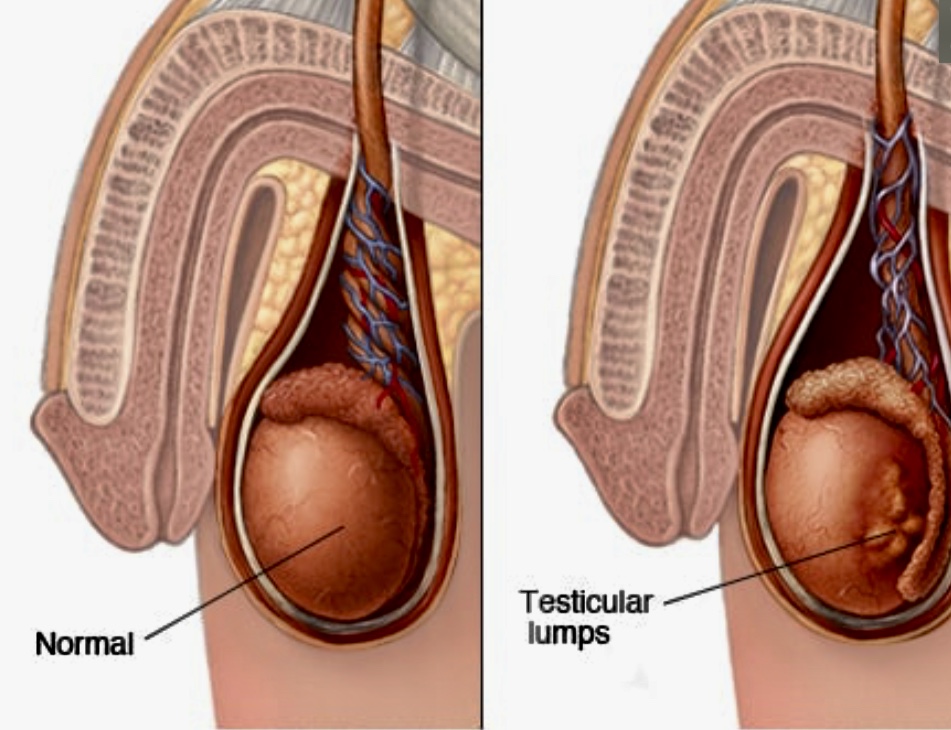
Mayo Clinic
Choriocarcinoma is a very rare and aggressive type of testicular cancer in adults. Pure choriocarcinoma is likely to spread rapidly to distant organs of the body, including the lungs, bones, and brain.
“The cause of testicular cancer is not known, but men whose testes did not descend into the scrotum (having a health problem called cryptorchidism) by age 3 have a greater chance of developing the disease than do men whose testes descended by that age,” the Merck manual says.
Cryptorchidism is best corrected surgically in childhood. “Sometimes, removal of a single undescended testis in adults is recommended to reduce the risk of cancer,” the Merck manual states.
It has been found that a family history of testicular cancer increases the risk of a man having it. If he has the disease, there is an increased risk that one or more of his brothers or sons will also develop it. But only a small number of testicular cancers occur in families. Most men with testicular cancer do not have a family history of the disease.
Symptoms
Most testicular cancers are found by men themselves. Self-examination of the testes is important for the early detection of testicular cancer. The most common method of early detection is performing a five-minute monthly exam while taking a shower.
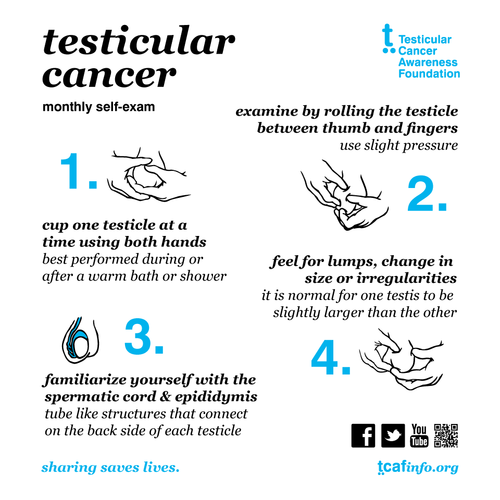
The website of the Testicular Cancer Awareness Foundation shares the following steps in testes self-examination:
Examine each testicle gently with both hands by rolling the testicle between the thumb and forefingers.
2. Find the epididymis, the soft tube-like structures behind the testicle that collects and carries sperm. If you are familiar with this structure, you won’t mistake it for an abnormal mass.
3. Look for any lumps or irregularities. Remember that lumps or bumps may also present themselves as painless.
4. Look for any changes in size, shape, or texture. Remember, it’s normal for one testicle to be slightly larger.
In some instances, testicular cancer is discovered by doctors during routine physical exams when examining the testicles. “Between regular check-ups, if a man notices anything unusual about his testicles, he should talk with his doctor,” urges www.medicinenet.com.
Even if testicular cancer has spread to other parts of the body, many men might not have symptoms right away, according to www.cancer.org. “Lower back pain can be a sign that the cancer has spread to the lymph nodes in the abdomen. Cancer that has spread to the lungs can cause trouble breathing (shortness of breath), chest pain, or a cough (sometimes with blood). Some cancers might cause abdominal pain, either from enlarged lymph nodes or metastasis (spread) to the liver. In rare cases, testicular cancer spreads to the brain and can cause headaches.”
A number of non-cancerous conditions, such as testicle injury or inflammation, can cause symptoms similar to those of testicular cancer. Inflammation of thetesticle (known as orchitis) and inflammation of the epididymis (epididymitis) can cause swelling and pain of the testicle. Both of these also can be caused by viral or bacterial infections.
Treatment
“The initial treatment for testicular cancer is surgical removal of the entire affected testis (radical orchiectomy). The other testis is not removed, so the man retains adequate levels of male hormones and remains fertile. Infertility sometimes occurs with testicular cancer but may subside after treatment,” the Merck manual informs.
With certain types of cancers, lymph nodes in the abdomen are also removed (retroperitoneal lymph node dissection) because cancer often spreads there first. Radiation therapy may also help, especially for a seminoma.
“A combination of surgery and chemotherapy often cures testicular cancer that has spread,” notes the Merck manual. “Blood levels of alpha-fetoprotein and human chorionic gonadotropin that were elevated at diagnosis decline after successful treatment.”
If levels rise after treatment, cancer may have recurred. “After surgery and any other necessary treatments are completed,” the Merck manual says, “a surgeon can replace the removed testis with an artificial one.”
According to the Merck manual, the prognosis for a man with testicular cancer depends on the type and extent of cancer. Almost all men with seminomas, teratomas, or embryonal carcinomas that are not widespread survive five years or more. Most men with cancer that have spread survive years or more. However, very few men with choriocarcinomas, which are spared rapidly, survive even five years.

