by Henrylito D. Tacio
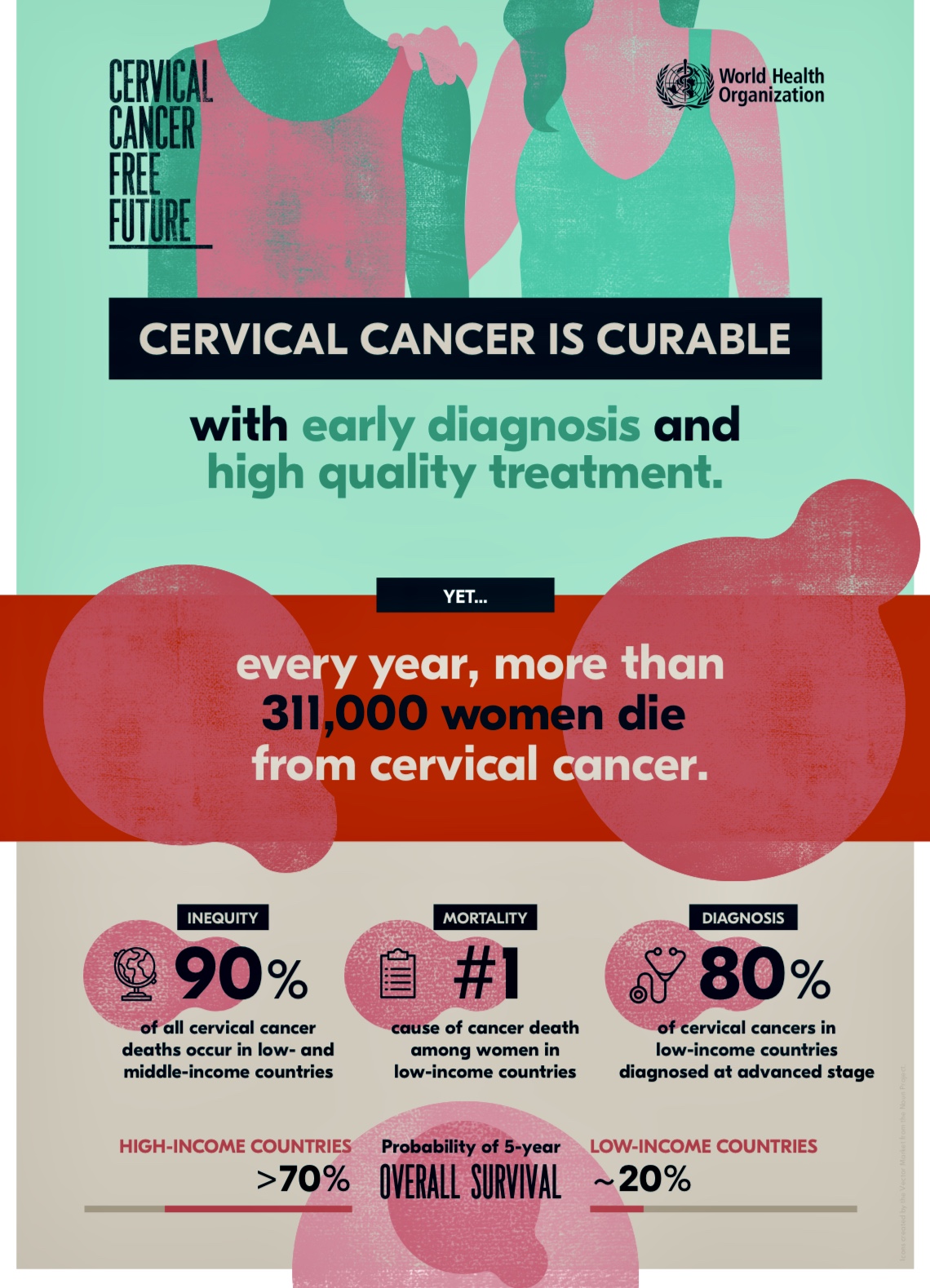
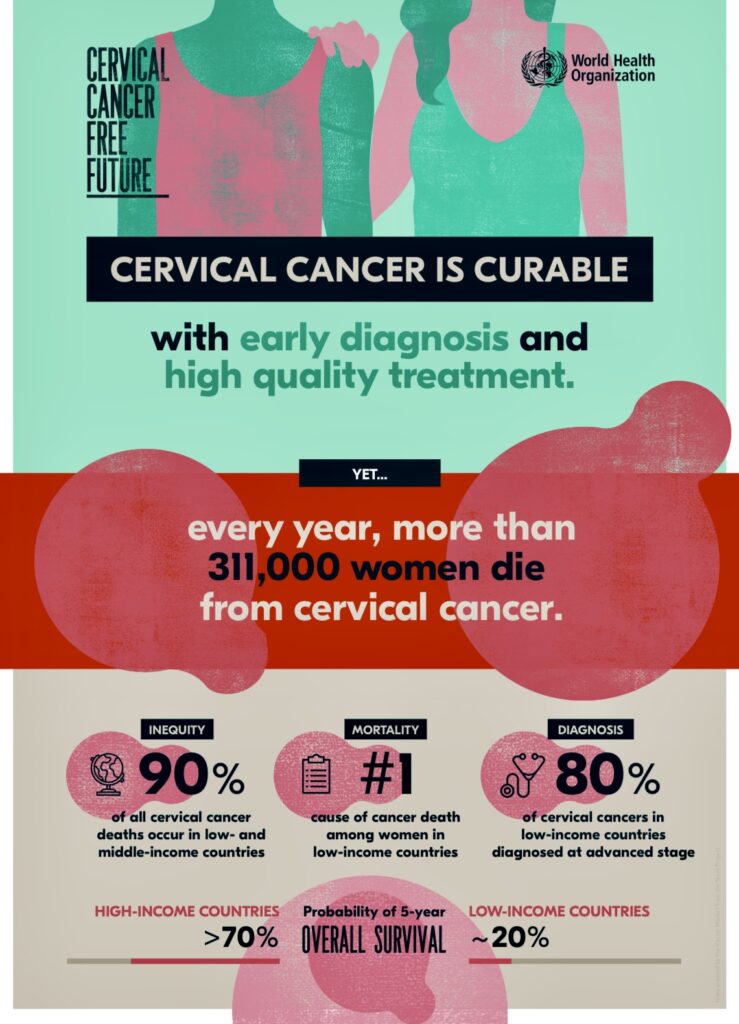
A world without cervical cancer is possible, according to the Geneva-based World Health Organization (WHO).
“Eliminating any cancer would have once seemed an impossible dream, but we now have the cost-effective, evidence-based tools to make that dream a reality,” said Dr. Tedros Adhanom Ghebreyesus, WHO Director-General. “But we can only eliminate cervical cancer as a public health problem if we match the power of the tools we have with unrelenting determination to scale up their use globally.”
Cervical cancer is a preventable disease. The WHO points out that it is also curable if detected early and adequately treated. Yet it is the fourth most common cancer among women globally.

“Without taking additional action, the annual number of new cases of cervical cancer is expected to increase from 570,000 to 700,000 between 2018 and 2030, while the annual number of deaths is projected to rise from 311,000 to 400,000,” the WHO says in a statement released during the launching of the Global Strategy to Accelerate the Elimination of Cervical Cancer last November 17.
In low- and middle-income countries, the WHO adds, the incidence of cervical cancer is nearly twice as high and its death rates three times as high as those in high-income countries.
“The huge burden of mortality related to cervical cancer is a consequence of decades of neglect by the global health community. However, the script can be rewritten,” says Dr. Princess Nothemba (Nono) Simelela, WHO Assistant Director-General. “Critical developments include the availability of prophylactic vaccines, low-cost approaches to screening and treating cervical cancer precursors; and novel approaches to surgical training.”
She said that through a shared global commitment to the Sustainable Development Goals and leaving no-one behind, the world’s countries are forging a new path to ending cervical cancer.

“Today’s development represents a historic milestone because it marks the first time that 194 countries commit to eliminating cancer – following adoption of a resolution at this year’s World Health Assembly,” WHO says.
Meeting the following targets by 2030 will place all countries on the path toward elimination: 90% of girls fully vaccinated with the HPV vaccine by 15 years of age; 70% of women screened using a high-performance test by age 35 and again by 45; and 90% of women identified with the cervical disease receive treatment (90% of women with pre-cancer treated and 90% of women with invasive cancer managed).
The United Nations health agency is recommending vaccination to those between the ages of 9 and 14.
Prevention of cervical cancer should start early – before girls are exposed to human papillomavirus (HPV). “The vaccine provides up to 95% coverage against cervical cancer,” Dr. Chia Yin Nin, a gynecologic oncologist practicing at Gleneagles Hospital in Singapore, told Business World.
Cervical cancer is the second leading cancer site among Filipino women, the Department of Health (DOH) reports. Every year, an estimated 7,277 new cases are reported, with 3,087 deaths. In recent years, however, more cases and more deaths are being reported.
The cervix is part of the female reproductive system located at the junction of the vagina and the uterus (womb). It is often called the neck of the womb. “Generally, all women who have had sexual intercourse are at risk of cervical cancer,” DOH states. “However, rare types of cervical cancer can occur even in women who never had any sexual intercourse in their life.”
In recent years, however, there has been overwhelming evidence that HPV causes cancer of the cervix. HPV takes several forms, which are referred to by number. “There are about 100 types of HPV that generally infect people in various parts of the body, but there are only 13 types that can cause cancer in the cervix,” wrote Dr. Cecilia Ladines-Llave in a paper presented at the Global Conference on Low-Resource Setting Cervical Cancer Prevention held at the Johns Hopkins University.
The most common causes of cervical cancer are HPV types 16 and 18. These two types are responsible for 70 percent of cervical cancer around the world. HPV Type 16 also causes oropharyngeal cancer. Condoms do not fully protect against infection because the virus can exist throughout the genital area and around the anus.
“We realize that, although HPV is sexually transmitted, it is not a sexually transmitted disease,” Dr. Nin explained. “It can be acquired through personal contact like fondling, petting, and sexual intercourse.”
The following had been established as possible causes of cervical cancer:
- Have had multiple sexual partners.
- Have had sexual partners (regular or casual) who themselves had several sexual partners.
- Have had a sexual partner who is infected with HPV and have had first sexual intercourse at a very early age, possibly 15 or 16 years old.
The risk of developing cervical cancer is increased by smoking, long-term use of oral contraceptives, a weakened immune system, and a family history of cancer, especially cervical cancer.
HPV is so prevalent in the community, and almost all women can have it. However, there are many forms of HPV, and many do not cause problems. “HPV infections usually clear up without any intervention within a few months after the acquisition, and about 90% clear within 2 years,” the United Nations health agency says. A small proportion of infections with certain types of HPV can persist and progress to cervical cancer.
Dr. Llave, the director of Cervical Cancer Prevention Network, was quoted as saying by Philippine News Agency (PNA) that 99.7% of cervical cancers are caused by HPV.
It takes 10 to 30 years of incubation before HPV infection becomes symptomatic. “There are no signs and symptoms about 18% of the time,” Dr. Llave stated. “Most women don’t go to the health centers unless they’re bleeding profusely, and they experience too much pain.
For about 20% of the women who are infected with HPV, cervical cancer may develop. “It is only when cancer develops that you experience the signs like bleeding during intercourse, bleeding between menstrual periods, or bleeding after menopause,” Dr. Nin said. “The patient can also experience other symptoms like back pain, cough, and swelling in the abdomen or limbs if cancer has spread.”
When detected early, cervical cancer, however, is curable. However, an ounce of prevention is better than a pound of cure, so goes a saying. Currently, 3 vaccines protect against HPV 16 and 18, which are known to cause at least 70% of cervical cancers. The third vaccine protects against three additional HPV types, which cause a further 20% of cervical cancers.
“The fight against cervical cancer is also a fight for women’s rights: the unnecessary suffering caused by this preventable disease reflects the injustices that uniquely affect women’s health around the world,” says Dr. Princess Nothemba Simelela. “Together, we can make history to ensure a cervical cancer-free future.”
Photos courtesy of WHO (World Health Organization)