By Henrylito D. Tacio
Photos sourced from different sources
Colon cancer is deadly!
Chadwick Boseman, who catapulted to fame when he starred in Black Panther, was diagnosed with cancer in 2016 – by that time, it was already in stage III. Despite treatments that included surgeries and chemotherapy, cancer progressed to stage IV.
But like a “true fighter,” he continued making movies despite battling the disease. Among those he did were Black Panther, Marshall, 21 Bridges, Da 5 Bloods, and Ma Rainey’s Black Bottom (for which he was honored with an Oscar). He died as a result of complications related to colon cancer at his home on August 28, 2020.
Between Christmas 2007 and New Year 2008, former president Corazon Aquino was not feeling well due to an episode of high blood pressure. But she had difficulty in breathing which was followed by fever. She was brought to the hospital, but she felt no better. In fact, “she developed a cough, lost her appetite, and noticeably lost weight.”
After several check-ups and tests on her health condition, the doctors came with a diagnosis: colon cancer. It wasn’t until on March 24, 2008, that the family disclosed to the public, through a televised statement, that the ex-president had colon cancer. She finally succumbed to the disease on August 1, 2009.
But when discovered early, colon cancer can be beaten. Early in his second term, American president Ronald Reagan felt something wrong inside his stomach. When he went to the hospital for a check-up, the doctors found growth in his large intestine.
Source American Cancer Society 
The doctors removed the polyp and nearly two feet of the intestine. His public experience helped to raise awareness about this type of cancer. Although he defeated the disease, Alzheimer’s disease claimed his life at the age of 93.
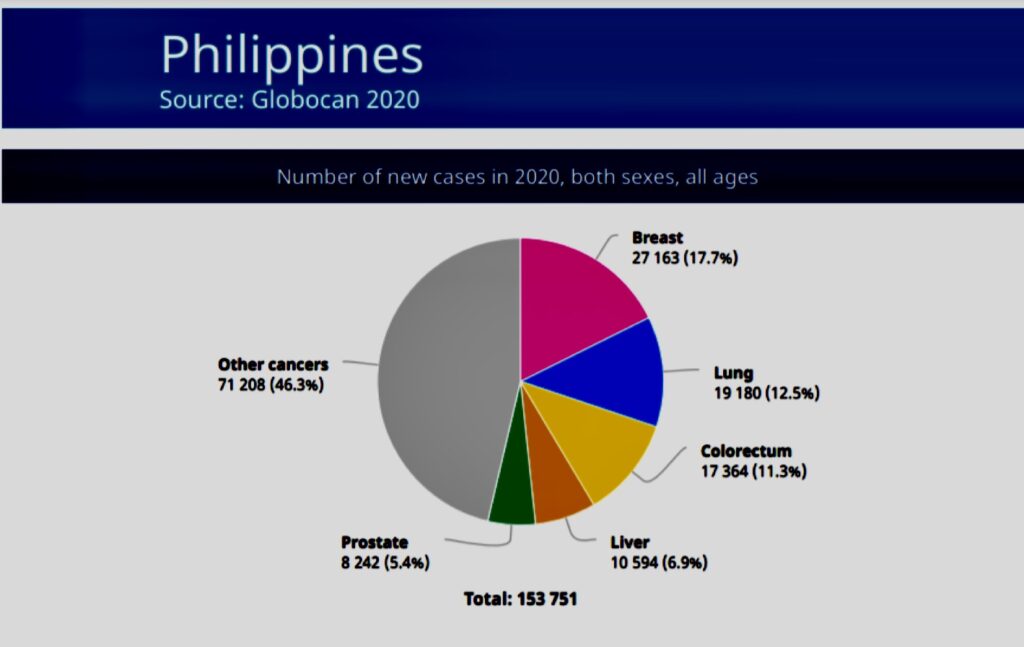
Colon cancer is the more common name, but this type of cancer also includes rectal. Thus it is called colorectal (CRC). And CRC has dislodged liver cancer as the number one gastrointestinal cancer in the Philippines.
CRC is fast becoming a leading cause of deaths in the country. The Global Cancer Observatory reported that in 2020, the number of Filipinos having CRC was 17,364.
“After food is chewed and swallowed,” states the American Cancer Society (ACS), “it travels to the stomach. There it is partly broken down and sent to the small intestine.” The small intestine is the longest part of the digestive system – about 20 feet.
“The small intestine also breaks down the food and absorbs most of the nutrients. It leads to the large intestine (also called the large bowel or colon),” explains the ACS. “The colon absorbs water and nutrients from the food and also serves as a storage place for waste matter. The waste matter moves from the colon into the rectum, the last 6 inches of the digestive system. From there, the waste passes out of the body.”
Source Glocan 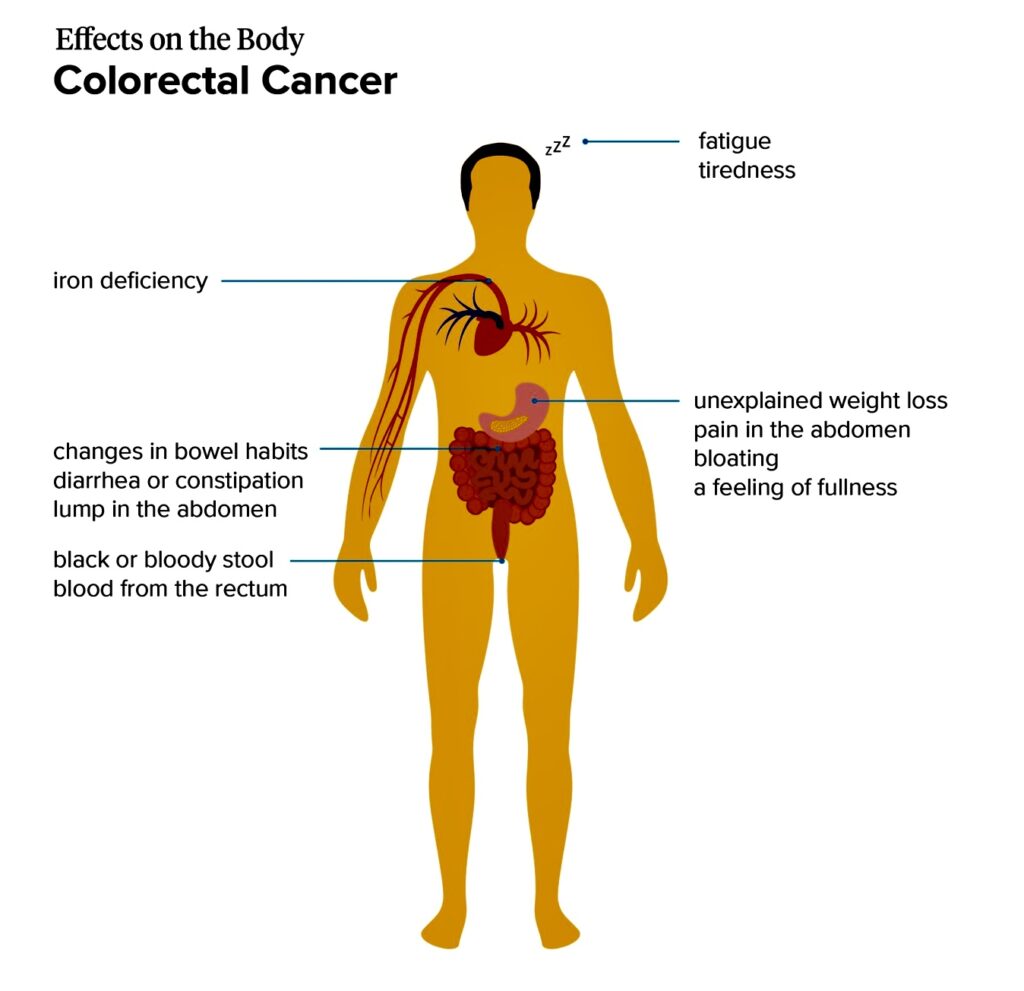
Source Medical News Today
Cancer that starts in any of these areas may cause different symptoms. Another common thing between colon cancer and rectal cancer is that, depending on where they start, the cancers develop slowly over many years.
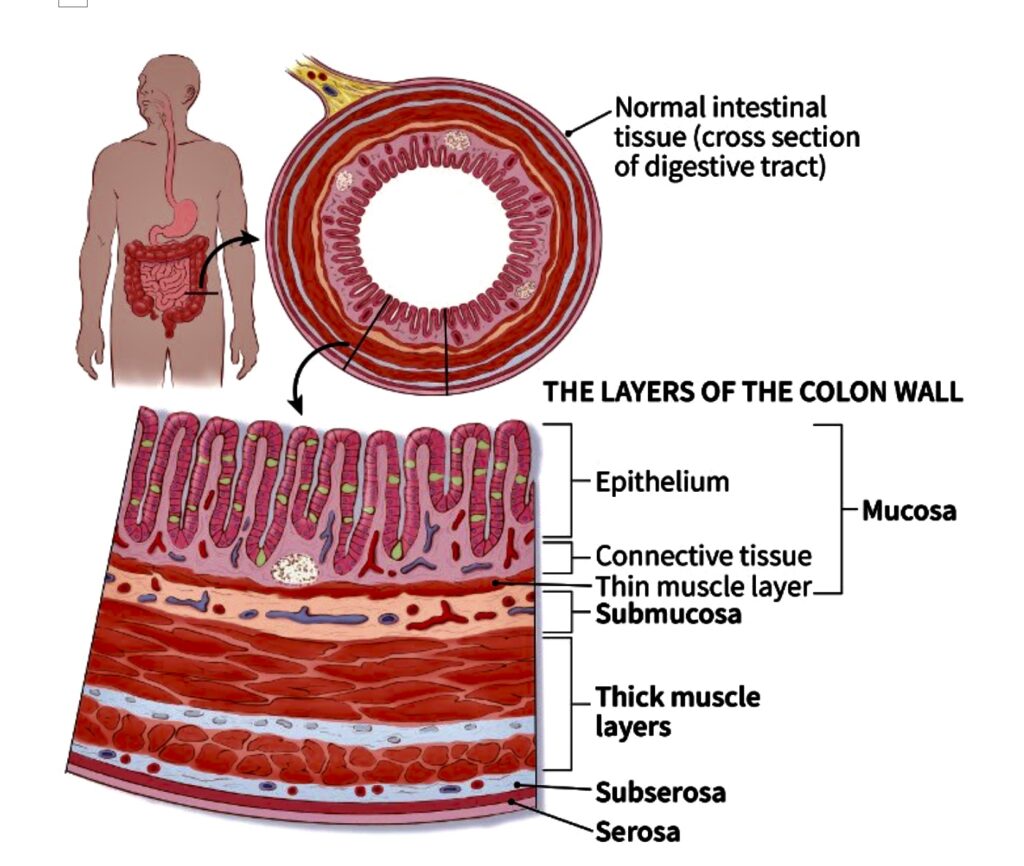
Most CRCs start as a growth on the inner lining of the colon or rectum. These growths are called polyps. “If cancer forms in a polyp, it can grow into the wall of the colon or rectum over time,” the ACS states. “The wall of the colon and rectum is made up of many layers. CRC starts in the innermost layer and can grow outward through some or all of the other layers.
“When cancer cells are in the wall, they can then grow into blood vessels or lymph vessels (tiny channels that carry away waste and fluid). From there, they can travel to nearby lymph nodes or to distant parts of the body.”
No one knows what causes CRC. “Epidemiologic, human case-control, and animal studies support a strong association between colon cancer and a diet that has high-fat (usually saturated fat), low fiber, and high red meat consumption,” Dr. Jun Ruiz, a gastroenterology consultant at St. Luke’s Medical Center and a diplomate of the American Board of Internal Medicine in Gastroenterology and of the Philippine College of Physicians in Internal Medicine.
Risk factors that predispose a person to develop colon and rectal cancer include age, personal history of adenoma or carcinoma, family history of CRC, and pre-existing diseases, like inflammatory bowel disease.
“Age 50 is the most common risk factor for CRC as 90% of cancers occur after the age of 50,” said Dr. Ruiz. As the Department of Health (DOH) puts it: “Colon cancer increases markedly after age 50.”
Several lifestyle-related factors have been linked to colorectal cancer. These include smoking, obesity, lack of physical activity, and alcohol intake.
In the past, CRC has been referred to as “a disease of the rich.” But such is not the case anymore. “(CRC) is more common in richer countries, but its incidence is rising in some developing countries,” the Geneva-based World Health Organization (WHO) reports. “The risk of developing those cancers that are typical of higher socioeconomic groups – cancers of the breast, colon, and rectum – can be expected to increase with economic development.”
CRC tends to grow slowly and may be asymptomatic for years, according to Dr. Ruiz. “Afflicted persons often have occult blood loss from their tumors, before they complain of symptoms. They can present with rectal bleeding and anemia, leading to fatigue, shortness of breath, and weight loss,” he says.
Dr. Ruiz says cancers of the right colon tend to grow larger than those of the left colon before symptoms occur. “Obstructive symptoms, like colicky abdominal pain, vague abdominal discomfort, change in bowel habits or stool caliber, and constipation, are found in advanced cases,” he adds.
Early detection of the dreaded disease can be achieved by screening tests. “CRC screening has resulted in reduction of related mortality up to 60-70%,” Dr. Ruiz says. “All methods have been proven to be cost-effective.”
Colonoscopy is the gold standard for CRC screening as it can detect and remove pre-cancerous polyps. “The procedure involves a flexible fiber-optic scope with a camera that is inserted through the rectum and is carefully advanced to visualize the colon under mild anesthesia,” explains Dr. Ruiz.
In the Philippines, colonoscopy can cost between P15,000 to P30,000, depending on the hospital.
Some patients may not want to have an invasive test. A stool test called FIT is a good screening alternative and is not expensive (it costs less than P500). “(FIT) detects only human blood and is specific for bleeding in the colon,” Dr. Ruiz states. “The test is repeated every year if the initial test is negative. If the test is positive, a colonoscopy is needed to rule out the presence of cancer.”
As a gastroenterologist who advocates colorectal cancer screening, Dr. Ruiz recommends a screening colonoscopy in individuals between 50 to 75 years of age who are relatively healthy and wherein the benefits of a colonoscopy outweigh the risks associated with the procedure.
“The patient has to understand that it requires a rigorous bowel preparation, and has more risks compared to the other alternative,” he explained. “The FIT is recommended to patients who may be at high risk for complications of a colonoscopy, or not willing to undergo a colonoscopy yet because of a variety of reasons.”
Colon cancer is deadly – but beatable if only it is discovered early. “The key here is screening patients who are already at risk for colon cancer, including patients who are 50 years or older,” Dr. Ruiz points out. “Patients may already have early cancer, even if they have no symptoms. We can also reduce the risk of colon cancer by removing pre-cancerous lesions (polyps) during a colonoscopy. In the end, CRC screening can just save your life or the life of a loved one.”

