Text by Henrylito D. Tacio
Photos: onhealth.com, iStock
A high school teacher, a municipal councilor, a government employee, and a bank teller. They may come from different academic backgrounds, but they had one thing in common: all of them died of breast cancer.
The high school teacher was in her late 40s when she died, leaving two sons behind. The municipal councilor was healthy when last seen by her colleagues, but after she filed a leave of absence, people were wondering. Months later, they learned that she had passed away.
Many of her office mates were bothered when the government employee was losing weight. She told them that she was “on a diet.” So, when her son reported that his mother died, many were caught by surprise. As for the bank teller, many were wondering why they could no longer see her. The clienteles were told that she died a month ago of breast cancer.
In a study, “Frequency of Cancer in Davao City,” conducted by the Philippine Science High School Southern Mindanao Campus, it was found that breast cancer is the second most reported cancer – after leukemia.
Based on data from the Southern Philippine Medical Center (SPMC), breast cancer had been diagnosed in 99 persons. In comparison, 125 people were diagnosed with leukemia.
One out of 13 Filipinas develop breast cancer, said the social media account of San Pedro Hospital Breast Cancer. Early detection and expert treatment are the woman’s best options to beat the disease.
In 2017, the Philippine Obstetrical and Gynecological Society listed the Philippines as having the “highest prevalence of breast cancer.”
“Despite the efforts in campaigning for breast cancer in the Philippines, there are still a lot of people who lack awareness and the proper knowledge of the disease,” deplores the Philippine Foundation for Breast Cancer, Inc.
No one should die of breast cancer as it is preventable. But the Geneva-based World Health Organization (WHO) says the vast majority of women with breast cancer in poor countries are diagnosed only after cancer has reached a late, untreatable stage.
“Many Third World women are unaware that they are at risk of breast cancer and do not know how to examine themselves for signs of the disease,” the United Nations health agency says.
Health experts agree that it is women themselves who can do something to detect the disease and prevent it from reaching an incurable stage. “Women can do breast self-examination (BSE) a week after menstruation,” the Philippine Cancer Control Program of the health department states.
The BSE can be done while under the shower, before going to bed at night, or upon waking up in the morning. A powder or soap over the breast may be used to make the examination easier. If married, a husband can help her in the breast examination. Any mass felt should lead to a physician.
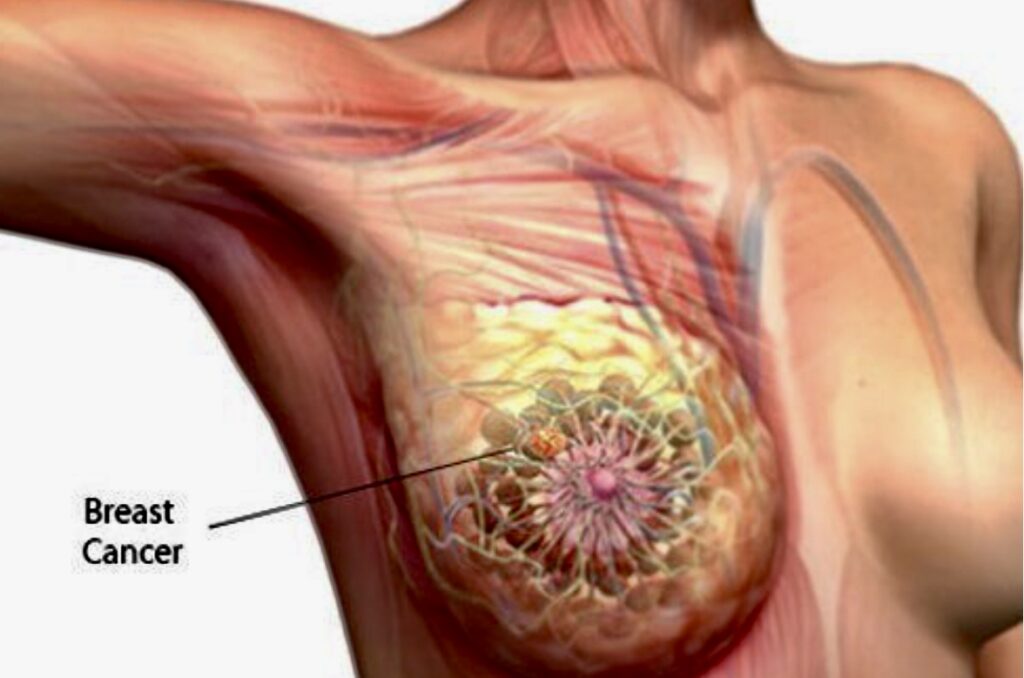
In the early stages, breast cancer usually has no symptoms. As a tumor progresses, a woman may experience pain or tenderness in her breast. She may also observe swelling in the armpit. But the most apparent symptom is a lump in the breast.
Aside from lump, other indicators include a noticeable or indentation on the breast; a change in the contour, texture, or temperature of the breast; a change in the nipple, such as an indrawn or dimpled look, itching or burning sensation; and unusual discharge from the nipple that may be clear, bloody, or another color.
The earlier a cancerous lump is detected and removed, the bigger the chances of treating it says Dr. Antonio Villalon, an oncologist at the Manila Doctors Hospital. He advised that between 20 and 39 years old, every woman should have a clinical breast exam every three years, and after age 40, every woman should have a clinical breast exam done each year.
Mammograms — a type of X-ray — are the chief way now to check for breast cancer. However, a radioactive tracer that “lights up” cancer hiding inside dense breasts showed promise in its first big test against mammograms, revealing more tumors and giving fewer false alarms. The experimental method — molecular breast imaging (MBI) — would not replace mammograms for women at average risk of the disease.
But it might become an additional tool for higher-risk women with a lot of dense tissue that makes tumors hard to spot on mammograms, and it could be done at less cost than magnetic resonance imaging, according to the Mayo Clinic in Rochester, Minnesota, which has been working on it for six years.
Right now, medical science is still baffled with what causes breast cancer. “Many different things can affect your chances of getting breast cancer,” states Breast Cancer Now (BCN), a London-based charity foundation. “There’s no single cause. It results from a combination of the way we live our lives, our genes and our environment. We can’t predict who will get breast cancer.”
But one thing is sure: Getting older is the most significant risk for developing breast cancer.
Another significantly higher risk is history. “A woman’s risk for breast cancer is higher if she has a mother, sister, or daughter (first-degree relative) or multiple family members on either her mother’s or father’s side of the family who have had breast or ovarian cancer,” the US Centers for Disease Control and Prevention (CDC) states. “Having a first-degree male relative with breast cancer also raises a woman’s risk.”
Personal history is another matter. “A woman with a history of cancer in one breast, such as ductal carcinoma in situ or invasive breast cancer, is three to four times likelier to develop a new breast cancer, unrelated to the first one, in either the other breast or in another part of the same breast,” webMD.com says.
Now, the good news. In 2018, Avon Philippines partnered with SPMC in setting up a breast clinic inside the government-owned hospital. “We want to create awareness on the importance of early protection and detection against breast cancer,” said the Avon official.
The partnership was lauded by Dr. Leopoldo J. Vega, then SPMC chief. He said that with an additional ultrasound machine, the center would be able to cater to up to 50 patients a day for breast cancer diagnostics.

