By Henrylito D. Tacio
“It is bad enough that people are dying of AIDS, but no one should die of ignorance.” – Elizabeth Taylor, American actress
***
At the height of coronavirus disease 2019 (COVID-19), people were paranoid of going to hospitals. And if ever they did, there were so many protocols to be followed before they could be admitted.
Health services were also greatly affected. It’s not only those health problems related to heart, mental, and respiratory but even those infectious diseases like tuberculosis (TB) and human immunodeficiency virus (HIV), the microorganism that causes acquired immune deficiency syndrome (AIDS).
“It is without a doubt that the COVID-19 pandemic has affected HIV work, both in the laboratory and the clinical setting,” admits Dr. Louie Mar Gangcuangco, a Filipino doctor who’s a tropical medicine specialist and senior preventive medicine resident at the Griffin Hospital-Yale School of Public Health in Connecticut, United States.
“In several institutions globally, laboratory work slowed down, with a decreased number of researchers performing experiments and taking turns in the laboratory to ensure social distancing,” adds Dr. Gangcuangco, who has worked as a researcher at the Hawaii Center for AIDS.
At the time when the pandemic was at its peak, many clinical staff had to focus on caring for COVID-19 patients. “Patients were encouraged to stay home for ‘non-urgent’ concerns, which unfortunately includes delaying HIV testing,” says Dr. Gangcuangco, adding that it was not unique only to HIV testing but also affected other services such as routine cancer screening.
Davao City was not spared from such a predicament. Dr. Jordana P. Ramiterre, head of the Reproductive Health and Wellness Center, told SunStar Davao that “the restrictions of the COVID-19 pandemic affected their office’s delivery programs and services to prevent HIV/AIDS.”
She added that treatment, care, and support to people living with HIV were greatly suffered, especially during the enhanced community quarantine, where people were required to stay at home and movements were restricted.
In 2021, a total of 12,341 new HIV infections were diagnosed in the country, based on a report released by the Philippine News Agency. This was up by 54% from the 8,036 new cases detected the previous year. “This number (of HIV cases) is tricky to interpret,” Dr. Gangcuangco says.
“We need to find out how many people were actually tested for HIV in 2020 and how many people were tested in 2021,” he explains. “If you will review the data from the Department of Health, only 254 people were newly diagnosed to have HIV in April 2020, compared to the 1,119 people diagnosed with HIV in April 2021.
“Since in 2020, people’s mobility was decreased and many were encouraged to stay indoors, it is likely that fewer people got tested for HIV during that time (and hence, the number of new detected HIV cases was lower),” he continues. “We also do not know how the pandemic affected people’s sexual risk behavior. This needs further research to answer.”
Early this year, the HIV/AIDS and ART Registry of the Philippines (HARP) of the health department said there were 875 confirmed HIV-positive individuals in January 2020. The National Capital Region topped had the most number of newly reported cases with 285 cases (33%), followed by Region 4A or Calabarzon with 156 cases (18%), and then Central Luzon with 100 cases (11%).
Western Visayas came fourth with 65 cases (7%). Davao and Central Visayas are tied with 50 cases each. All in all, these top regions comprised 81% of the total number of cases in January 2020.
Of the total reported cases, 99% (863) were infected through sexual contact: male-male sex, male-female sex, and sex with males and females. The male-to-male registered the highest number: 592 cases.
Less than one percent (3) of the reported cases each have acquired HIV through sharing of infected needles and through mother-to-child transmission.
What is alarming is that 32% of the new cases involved young people. About 283 of the reported cases were among those 15-24 years old, and 96% (272) were male. Some 69 of these youths were in advance infection of HIV. Ninety-nine percent of the cases were infected through sexual contact.
This phenomenon is not confined to the Philippines alone. “Majority of people newly diagnosed with HIV are among persons between 25 and 34 years old,” Dr. Gangcuangco says. “This is likely driven by the higher risk of sexual behavior within this age group. The accessibility of casual sex through online platforms is also likely contributing to the increased incidence of HIV in this age group.”
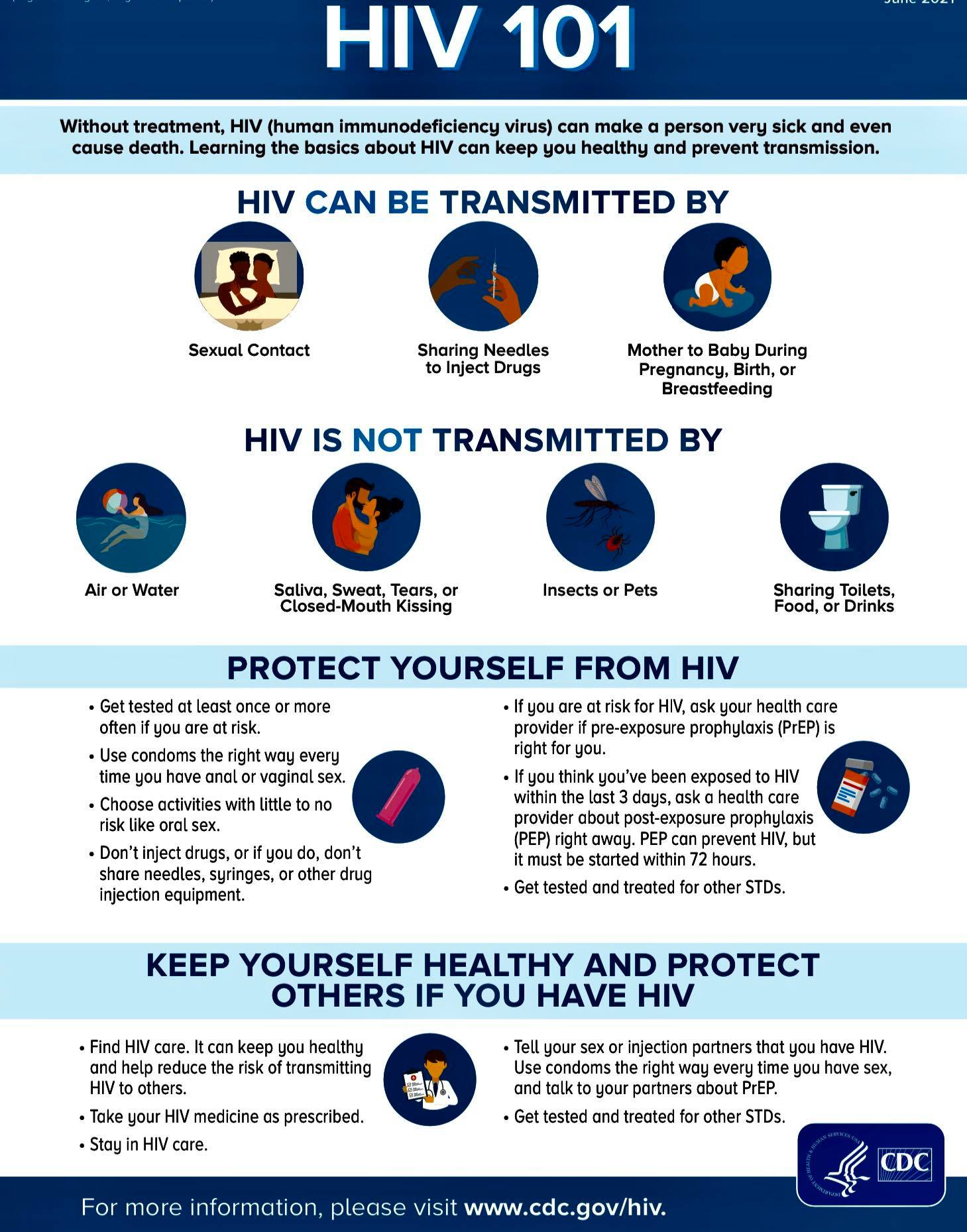
HIV respects no one; it spares no one. HIV, a virus that damages the immune system, is primarily acquired through unprotected sex from an infected partner. “The highest risk is through male-to-male receptive anal sex,” Dr. Gangcuangco explains. “Regardless of gender identity, high-risk behavior include sex without a condom, having multiple sexual partners, sex under the influence of alcohol or drugs, and sex in exchange of goods or favor.”
Aside from sex, HIV can also be transmitted through sharing of needles among people who inject drugs. HIV can be passed from mother to child if the mother’s HIV viral load is not controlled.
How will you know you are infected with HIV? “Some people have flu-like symptoms within 2 to 4 weeks after infection,” says the US Centers for Disease Control and Prevention (CDC). “These symptoms may last for a few days or several weeks.”
Possible symptoms include fever, chills, rash, night sweats, muscle aches, sore throat, fatigue, swollen lymph nodes, and mouth ulcers. “But some people may not feel sick,” the CDC states. “These symptoms don’t mean you have HIV. Other illnesses can cause these same symptoms.”
These days, being infected with HIV is no longer a death sentence. “HIV is not and should not be a death sentence anymore,” points out Dr. Gangcuangco. “If HIV is detected early and if the patient takes antiretrovirals early, the virus can be controlled.”
However, in order to be treated, you need to know if you have HIV. And you will only find out if you undergo HIV testing. “Testing for HIV and other sexually transmitted infections is strongly advised for all people exposed to any of the risk factors,” said the World Health Organization (WHO) on its website. “This way, people learn of their own infection status and access necessary prevention and treatment services without delay.”
However, all HIV testing services must follow the five principles recommended by WHO: consent (informed), confidentiality, counseling, correct test results, and connection (linkage to care, treatment, and other services).
In Davao City, there are three facilities where people can go to be tested for HIV: Southern Philippine Medical Center in Bajada, Davao Doctors Hospital in Quirino Street, and Davao Reproductive Health and Wellness Center in Emilio Jacinto Street. In Tagum City, they can go to Davao Regional Medical Center in Apokon.
“HIV testing must be made accessible to everyone,” Dr. Gangcuangco urges. “The Philippines must develop the infrastructure to facilitate HIV self-screening using home-based kits. This would entail a telephone hotline for anyone who has questions about HIV or among those who might test positive using the screening test.
“Clinics must also be able to expand to accommodate HIV testing after office hours and during weekends,” he suggests. “Free HIV testing must be made available and accessible to those who could not afford it.”
According to Dr. Gangcuangco, knowing one’s HIV status is not just a right but also a responsibility. “People with HIV can live normal and productive lives as long as they take their medications and follow-up regularly with your doctor. Getting tested is not only for yourself, but also for your loved ones,” he says.
Dr. Gangcuango believes that educating the public on safe sex practices, such as the importance of condom use, is key to curbing the HIV epidemic in the country.
He suggests several changes in the health care system have to be made. Aside from having HIV testing accessible to all people, he also includes HIV treatment to be more available to everyone. “This includes training of medical practitioners on the appropriate care of people living with HIV,” he says. “Clinic hours should be expanded to ensure that those who work 8am to 5pm jobs can also access HIV testing and treatment outside of work hours.”
He also talks about pre-exposure prophylaxis. Better known as “PrEP,” it is a daily pill that people can take to prevent HIV. “PrEP is slowly being rolled out in the Philippines and its expansion would be a great addition to our armamentarium against HIV,” he says. “Among those who have HIV infection, ensuring that patients have enough social and clinical support so that they remain adherent to antiretroviral therapy is also very important.”
Right now, there is still no cure for HIV, but thanks to continuing medical advances in medications, HIV can now be seen as a chronic disease. In fact, people infected with HIV can enjoy long careers, get married, and raise families.
“There’s no cure for HIV, but treatment options are much better than they were a few decades ago,” Dr. Gangcuangco says. “Because of medical advancements, many people now live long, active lives with HIV.”
The medicines that treat HIV are called antiretroviral drugs. There are more than two dozen of them, and they fall into six main types. Each drug fights the virus in your body in a slightly different way.
Research shows that a combination of so-called “cocktail,” of drugs is the best way to control HIV and lower the chances that the virus becomes resistant to treatment. A doctor can recommend a patient to take three different medicines from two of the groups.
“Which specific ones your doctor prescribes depends on what other medical conditions you have or are likely to get, how well your immune system is working, and even how many pills you want to take each day,” WebMd.com says.
Once an HIV-infected person starts having treatment, he should not stop doing so. “Keep taking your HIV medications,” reiterates WebMd.com. “It’s dangerous to change how you’re taking them – or to stop altogether – if you’re unhappy with how you feel or how they affect you. That can make it easier for HIV to become resistant to drugs and harder to treat.
“Continuing treatment is the key to not only preventing the development of AIDS, but is key to maintaining a relatively normal lifestyle. It is possible, with the correct treatment, to obtain a normal life expectancy,” the website says.

