Text by Henrylito D. Tacio
Infographics: Wikipedia, Freepik
Photo: St. Luke’s Medical Center
It’s the time of the year when rain is common. As climate change is already affecting the country, the rains that come to Davao Region have become stronger and heavier. The result: floods.
Davao City, the country’s biggest metropolis in terms of land area, is not spared from such natural calamity. Houses are deluged, people living near the riverbanks are displaced, and the economy is greatly affected. But the aftermath is even worse: leptospirosis.
“Leptospirosis attacks during the rainy season when there are frequent floods,” says Dr. Elmer Alcaide Linao, a board-certified consultant in internal medicine, cardiology, and critical care at St. Luke’s Medical Center Heart Institute.
In Davao City, leptospirosis has been endemic, according to a health report. In 2013, an outbreak occurred after a flash flood. In 2013, the Department of Health (DOH) received a report on the increasing number of leptospirosis cases after the monsoon flooding.
In December 2017, tropical storm Tembin hit the region and caused flooding and landslides. In Davao City, a man experienced fever a few days after walking in the floodwater to save some belongings during the typhoon. The fever was accompanied by chills, vomiting, abdominal pain, diarrhea, jaundice, and calf pain. When he went to pee, he observed tea-colored urine in the bowl.
Leptospirosis outbreaks occur in the city, according to studies, because of the following: wading in floodwater, swimming in floodwater, having contact with moist soil, and having open wounds.
“During flooding, people stayed home to secure their properties but did not wear protective clothing nor cover their wounds,” one study found out.
Health officials think leptospirosis cases may surge again as a heavy downpour of rains that may cause massive flooding will continue to happen during the remaining months of the year.
Ounce of prevention
An ounce of prevention is better than a pound of cure, so goes a popular saying. “Just like what happened in the recent flooding, if you are wading through floodwaters you have to wear protective gear such as boots and wash your feet thoroughly with soap,” Dr. Ma. Theresa Bad-ang, a nephrologist, told Philippine News Agency.
Leptospirosis is a bacterial disease that plagues humans and animals. It was first described by Adolf Weil in 1886 as “acute infectious disease that causes enlargement of spleen, jaundice and nephritis.”
“Though a relatively bacterial infection in humans, leptospirosis breaks in the human body through skin ruptures, the eyes, or the mucous membranes that have come in contact with animal urine-contaminated water,” explains Dr. Linao.
Where to get it
Aside from floodwaters, a person can also get leptospirosis by contact with freshwater, damp soil, or vegetation contaminated by the urine of infected animals, especially rodents and dogs. Leptospirosis bacteria also enter the body when a person swallows contaminated food or water.
Filipinos may learn a lesson from this incident which happened in Texas, United States, some years back. A woman went boating one Sunday taking with her some cans of soft drinks, which she put into the refrigerator of the boat.
On Monday, she was taken to the hospital and placed in the Intensive Care Unit. She died on Wednesday. The autopsy concluded she succumbed to leptospirosis. This was traced to the can of soft drink she drank from, not using a glass. Tests showed that the can was infected by dried rat urine.
“It is highly recommended to thoroughly wash the upper part of all soft drink cans before drinking out of them,” the news report stated. “The cans are typically stocked in warehouses and transported straight to the shops without being cleaned.”
Now, read this alarming evidence: A study at New York City University showed that the tops of all soda cans are more contaminated than public toilets, that is, full of germs and bacteria.
Rats and other animals
“Rodents and other mammals can transmit the disease through their pees in stagnant waters like those in drainages, sewers, or even in garbage sites,” Dr. Linao says. “Domestic pets can carry the disease from these infected animals to unsuspecting victims inside the house through exposure to these places.”
Rats are the most dominant carrier as they are incontinent. “(Rats) may spread the disease through their urine,” Dr. Linao says. “In most cases, the bacteria die when the urine dries out but when they reach the water, they remain potent for a long time. Any damp areas where rats urinate can be contaminated.”
Rats and other “reservoir” species – cattle, pigs, sheep, and horses, to name a few – can either be in the infected or carrier state. “An infected animal could either recover or die from it. The carrier, however, may never have any symptoms of the disease but carries a colony of bacteria in the body.”
Signs and symptoms
Leptospirosis occurs between four to 10 days after exposure to the bacteria. Once in the bloodstream, the bacteria that causes leptospirosis can reach all parts of the body and cause signs and symptoms of illness. “Because mild leptospirosis typically causes vague, flu-like symptoms, many infections probably go unreported,” says The Merck Manual of Medical Information.
Studies have shown that leptospirosis causes mild disease in about 90 percent of infected people, whereas 10 percent have severe, potentially fatal, a disease that affects many organs. “If the victim survives, he still has to deal with kidney or liver failure,” Dr. Linao points out.
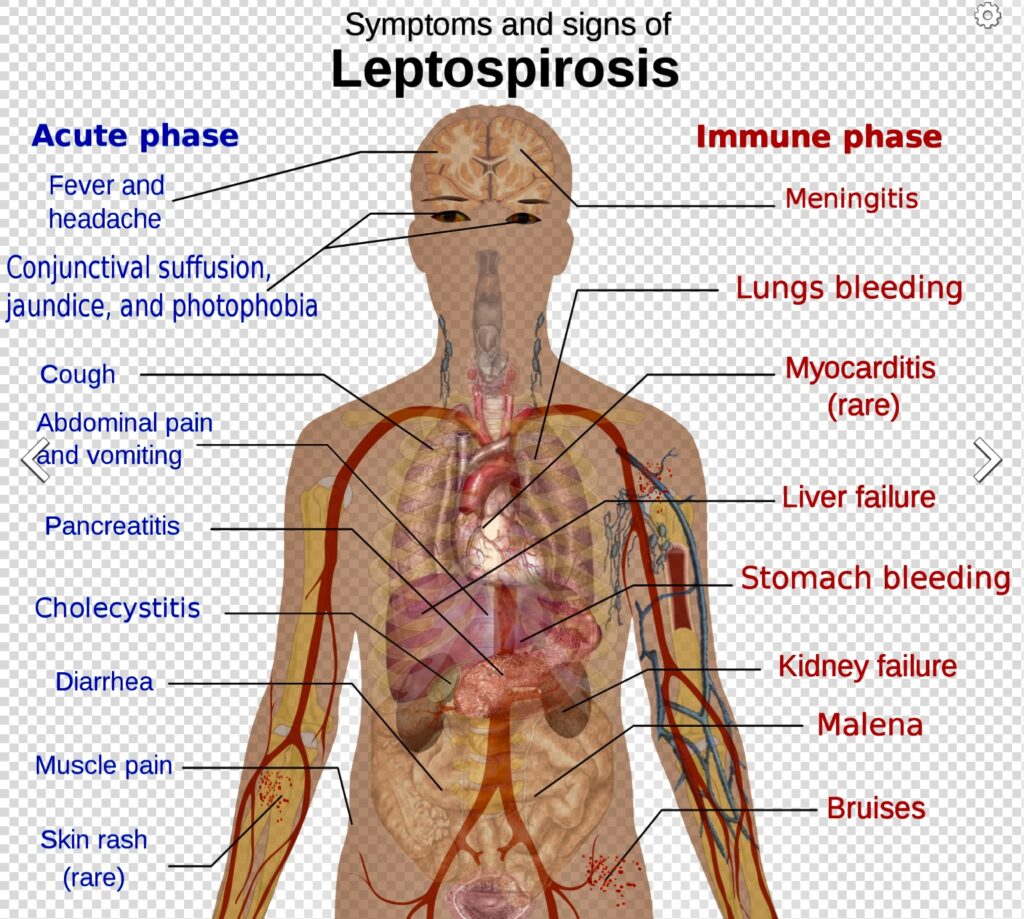
Actually, there are two phases of leptospirosis. “The first phase starts two to 20 days after infection with Leptospira,” the Merck manual informs. “Symptoms begin abruptly with a fever, headache, severe muscle aches, and chills. The eyes usually become red on the third or fourth day. Nausea and vomiting are common.”
Symptoms involving the lungs (including coughing up of blood) occur in 10 to 15 percent of infected people, studies reveal. Episodes of chills and fever, which often reach 102 degrees Fahrenheit, continue for four to nine days.
The fever clears for a few days, marking the beginning of the second phase. “During the second phase,” the Merck manual says, “the body’s immune reaction against the bacteria causes inflammation, producing many symptoms. The fever returns, and there is often inflammation of the tissues covering the brain (meningitis), causing a stiff neck, headache, and sometimes stupor and coma.
“In severe forms of the infection, people may also have inflammation of the liver, kidneys, and lungs, resulting in jaundice, kidney failure, and bloody cough. Sometimes the heart is inflamed, causing palpitations and dangerously low blood pressure (shock). A pregnant woman who develops leptospirosis may miscarry.”
The severe form of leptospirosis is called Weil’s disease, which causes a continuous fever, stupor, and a reduction in the blood’s ability to clot, leading to bleeding within tissues. “By the third to sixth day, signs of kidney damage and liver injury appear,” the Merck manual says. “Kidney abnormalities may cause blood in the urine and painful urination. Liver injury tends to be mild and usually heals completely.”
Diagnosis and treatment
Only a doctor can confirm the diagnosis of leptospirosis. The doctor does this by identifying Leptospira – the bacteria that causes leptospirosis – in cultures of blood, urine, or cerebrospinal fluid samples or, more commonly, by detecting antibodies against the bacteria in the blood.
According to the Merck manual, infected people who do not develop jaundice (yellowing of the skin and white of the eyes) usually recover. Jaundice indicates liver damage and increases the death rate to 10 percent or higher in people older than 60.
The US-based Centers for Disease Control and Prevention (CDC) suggests that antibiotic therapy (doxycycline or penicillin) should be administered by a medical practitioner to save the person from complications. These may be taken orally, but in severe infections, they may be given intravenously.
“It is imperative that an infected person see a doctor right away,” Dr. Linao suggests. “The large number of bacterial strains involved does not guarantee immunity even when the person has previous exposure to leptospirosis.”
Leptospirosis, unlike the coronavirus disease 2019 (COVID-19), is not a contagious disease. “People with the disease do not have to be isolated, but care must be taken when handling and disposing of their urine,” the Merck manual points out.

