Text by Henrylito D. Tacio
Photos: shutterstock, vectorstock.com, healthxchange.sg
It may be a disease of the past, but tuberculosis (TB) is still killing people – more than a million of them. In fact, TB deaths have increased for the first time in a decade as a direct result of the coronavirus disease 2019 (COVID-19) pandemic.
That’s according to the Geneva-based World Health Organization (WHO).
New data from the UN health agency highlighted how years of global progress in tackling the preventable disease had been “reversed” since the pandemic overwhelmed health care systems in 2020, preventing vulnerable people from seeking help.
Lockdowns had also stymied many people’s access to essential health care services. With this, the number of TB deaths “could be much higher in 2021 and 2022,” said the WHO’s 2021 Global TB Report.
“This report confirms our fears that the disruption of essential health services due to the pandemic could start to unravel years of progress against tuberculosis,” said WHO Director-General, Tedros Adhanom Ghebreyesus. “This is alarming news that must serve as a global wake-up call to the urgent need for investments and innovation to close the gaps in diagnosis, treatment and care for the millions of people affected.”
Globally, TB incidence is falling at about 2% per year, and between 2015 and 2020, the cumulative reduction was 11%. This was over halfway to the End TB Strategy milestone of a 20% reduction between 2015 and 2020.
Most feared
But the COVID-19 changes the scenario. Today, the WHO considers TB as “the second deadliest infectious killer after COVID-19.”
TB and COVID-19 may both be respiratory diseases, but there are differences. For one, TB is caused by bacteria, while COVID-19 is caused by a virus genetically related to the severe acute respiratory syndrome coronavirus called SARS-CoV-2. Both are spread through close physical contact.
“Tuberculosis spread usually in hours, and for COVID-19, it’s a virus with very short interaction, (which) results in the spread of the infection,” Dr. Shama Ahuja, director of TB Surveillance and Epidemiology at the New York City Department of Health and Mental Hygiene told USA Today.
But what worries experts is that COVID-19 could activate latent tuberculosis. “When people get sick with SARS-CoV-2, they could not only activate their latent TB, but also transmit their TB along with SARS-CoV-2 to others,” Prof. Faramarz Valafar of San Diego State University’s School of Public Health, who’s a genomics expert and TB researcher.
No wonder COVID-19 is the most feared disease these days, as there’s still no cure for it. In fact, the existence of the new coronavirus made it impossible to provide and access essential TB services, leaving many people undiagnosed in 2020.
In a worrying development, WHO noted that the number of newly diagnosed people with the disease fell from 7.1 million in 2019 to 5.8 million in 2020, meaning that far fewer people were diagnosed, treated, or provided with TB preventive treatment compared with 2019.
1.5 million deaths
Covering the response to the epidemic in 197 countries and areas, the TB report found that in 2020, some 1.5 million people died from TB in 2020 – more than in 2019.
The report cited 30 countries with the highest TB burden. In Asia, most TB cases are from Bangladesh, China, India, Indonesia, Myanmar, North Korea, Pakistan, the Philippines, Thailand, and Vietnam.
“Tuberculosis remains the biggest killer in the world,” says the Davao Doctors Hospital on its website, ddh.com.ph. “The Philippines ranks 8th in the world and third in the Western Pacific Region in terms of the burden of TB. It is the 6th cause of morbidity and mortality in our country with an estimated 270,000 cases detected every year.”
The Department of Health (DOH) said about 75 Filipinos die from TB each day – that’s about three people per hour.
Davao Region
In Davao Region, TB continues to be a health threat. In 2016, 13,330 cases were detected in the region. In the first two quarters of 2017, as many as 7,000 cases were already recorded by the regional TB program of the health department.
“Because of the advocacies, because more initiatives are being done under the program of the DOH, we are expecting more detected cases including the cases at the barangay level and the vulnerable groups,” Dr. Hansel Amoguis, the regional TB program medical coordinator, was quoted as saying by media.
TB is caused by bacteria called Mycobacterium tuberculosis that most often affect the lungs. Unlike cancer, TB is curable and preventable. The WHO says an estimated 66 million lives were saved through TB diagnosis and treatment between 2000 and 2020.
Ancient disease
TB, one of the oldest diseases afflicting mankind, is spread from person to person through the air. When people with lung TB cough, sneeze, or spit, they propel the TB germs into the air. A person needs to inhale only a few of these germs to become infected.
The WHO says about one-quarter of the world’s population has a TB infection, which means people have been infected by TB bacteria but are not (yet) ill with the disease and cannot transmit it.
People infected with TB bacteria have a 5–10% lifetime risk of falling ill with TB. Those with compromised immune systems, such as people living with HIV (human immunodeficiency virus), malnutrition or diabetes, or people who use tobacco, have a higher risk of falling ill.
When a person develops active TB disease, the symptoms (such as cough, fever, night sweats, or weight loss) may be mild for many months. This can lead to delays in seeking care and results in the transmission of the bacteria to others.
Infection to others
People with active TB can infect 5–15 other people through close contact over the course of a year. Without proper treatment, 45% of HIV-negative people with TB on average and nearly all HIV-positive people with TB will die.
The risk of active TB is also greater in persons suffering from other conditions that impair the immune system. People with undernutrition are three times more at risk. Globally in 2020, there were 1.9 million new TB cases that were attributable to undernutrition, the WHO reports.
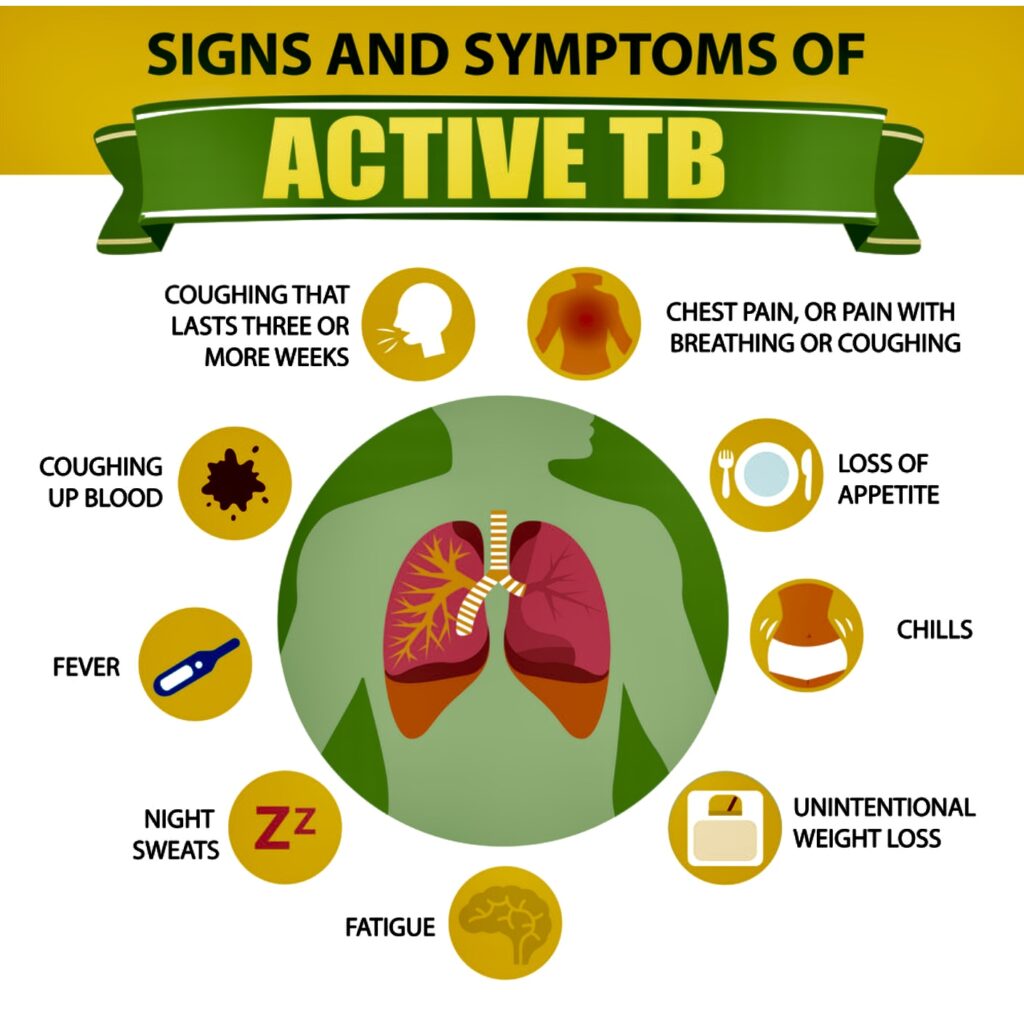
Signs and symptoms of TB 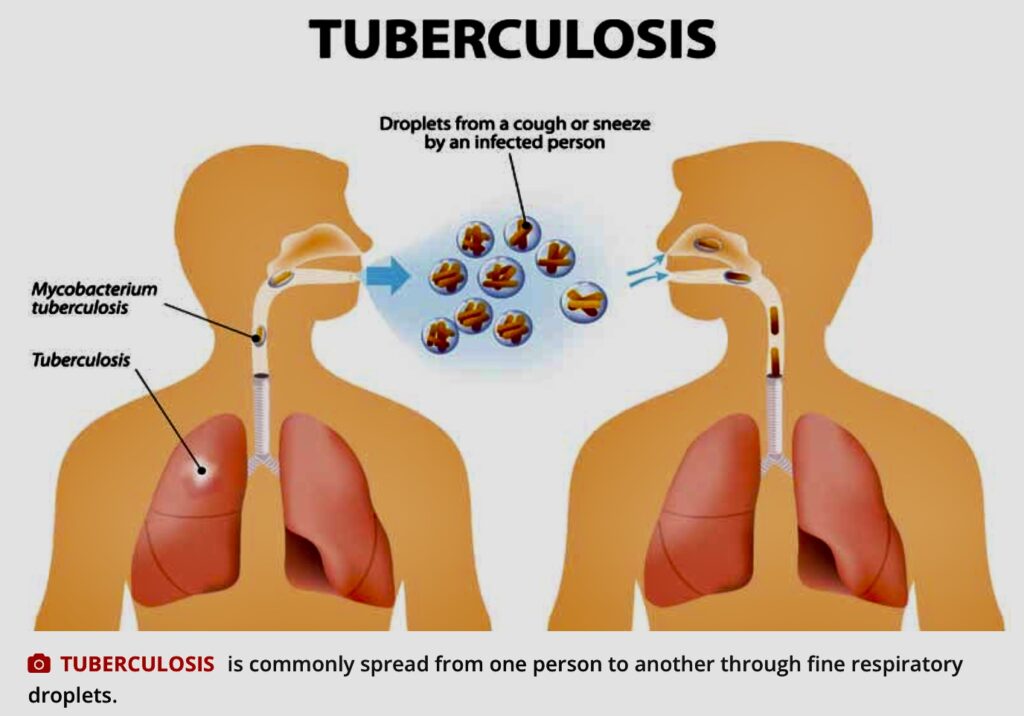
Transmission
Alcohol use disorder and tobacco smoking increase the risk of TB disease by a factor of 3.3 and 1.6, respectively. The WHO says 0.74 million new TB cases worldwide in 2020 were attributable to alcohol use disorder, and 0.73 million were attributable to smoking.
Drug regimen
But unlike COVID-19, TB is preventable and curable. About 85% of people who develop TB can be treated with a six-month drug regimen; treatment has the added benefit of curtailing onward transmission of infection.
If you are diagnosed with active TB, then you must absolutely take anti-TB medicines. “There are no ifs and buts,” says Dr. Willie T. Ong, who co-authored the book with his wife, Dr. Liza Ong, Doctors’ Health Tips and Home Remedies. “It’s for your own good and for the good of the people around you. If you don’t take the medications, then you will be infecting an average of 10 persons in a year, including your loved ones and children.”
According to Dr. Ong, the treatment for TB is a bit more complicated compared to ordinary infections “since it will take approximately 6 months to completely eradicate the bacteria.” In cases where the infection is serious, it may take about nine months of treatment.
Only a doctor can give you the correct treatment, so you better see one. “Never self-medicate,” Dr. Ong reminds. “This is the worst thing you can do. It will only strengthen the bacteria inside you and make you resistant in one tablet.”
Dr. Ong suggests that those who are undergoing treatment stay at home during the first three weeks of treatment. “Don’t go to school, work or come in close contact with people,” he says. “Your saliva and phlegm can infect others.”
He also recommends that they wear a face mask during the first three weeks of treatment. “Cover your mouth with a tissue when you cough, sneeze or laugh too hard,” Dr. Ong urges. “Then throw the tissue away in a sealed container.”
As a sort of reminder, all TB medications must be taken one hour before meals. “It is ideal not to break the dose of the drug,” Dr. Ong reminds. The patient needs to see his doctor to undergo blood tests to check for possible liver side effects of the drugs taken.
Side effects aren’t common, but some TB medicines can occasionally be harmful to the liver, he says. In addition, the color of the urine will change from yellow to orange. But don’t worry; the change of color is “a normal reaction to the treatment course.”
Dr. Ong suggests that you need to consult your doctor once you experience any of the following: nausea, vomiting, loss of appetites, yellowing of the skin, or fever of more than three days.
The most important thing: “Complete the 6- to 9-month course of your medicines,” Dr. Ong declares. “Do not stop your medicines without your doctor’s permission. Doing so will cause the TB bacteria to mutate and come back in a stronger and more virulent form.”
Multi-drug resistant TB
In 2011, the WHO regional office reported that about 10,600 Filipinos have multi-drug resistant TB (MDR-TB). By 2015, MDT-TB cases went to 15,000.
Health experts say “treatment outcomes for MDR-TB are typically worse than those for patients with drug sensitive TB, in significant part due to the length of treatment and the potential for adverse effects from second-line medications.”
The international community wants to end TB from this planet by 2030. After all, TB is preventable and curable. But in the Philippines, the number of people with TB continues to increase every year.
“Ending TB requires concerted action by all sectors and all care providers,” the WHO points out. “Everyone has a role to pay in ending TB – individuals, communities, businesses, governments, societies. Everyone must join the race to end TB by 2030.”
Meanwhile, the clock is ticking. It’s time to ensure that no one dies of TB anymore.

