Text by Henrylito D. Tacio
Photos: Wikipedia
Right now, the Philippines – just like the rest of the world – is focusing on its fight against the dreaded coronavirus disease 2019 (COVID-19), which has snatched the lives of almost 25,000 people already.
But there’s another disease that has been taking a toll among Filipinos since the time of President Manuel L. Quezon – who died from it. More deadlier than COVID-19, it’s tuberculosis (TB).
“Approximately, 74 Filipinos die of TB every year and is among the top 10 causes of death in the country,” says the Department of Health (DOH) on its website.
About one million Filipinos have active TB disease, according to the World Health Organization (WHO). “This is the third highest prevalence rate in the world, after South Africa and Lesotho,” said Dr. Gundo Aurel Weiler, director of the WHO Western Pacific.
The WHO envisions to end TB from the world by 2030. “Yet, the Philippines is among the few countries where the number of people with TB continues to increase every year,” Dr. Weiler deplored.
The current pandemic is fueling the disease. Today, many TB-affected individuals in the country dismiss getting checked due to the fear of contracting COVID-19. There is also a lack of education towards treatment. In addition, many Filipinos perceive TB as a low-risk disease.
Last year, the health department recorded a decline in TB cases. “We see this as a direct effect of the COVID-19 pandemic on a critical disease prevention and control program like TB,” said Health Secretary Francisco T. Duque III. “The quarantine has extremely affected and limited the health seeking behaviors of our fellow Filipinos.”
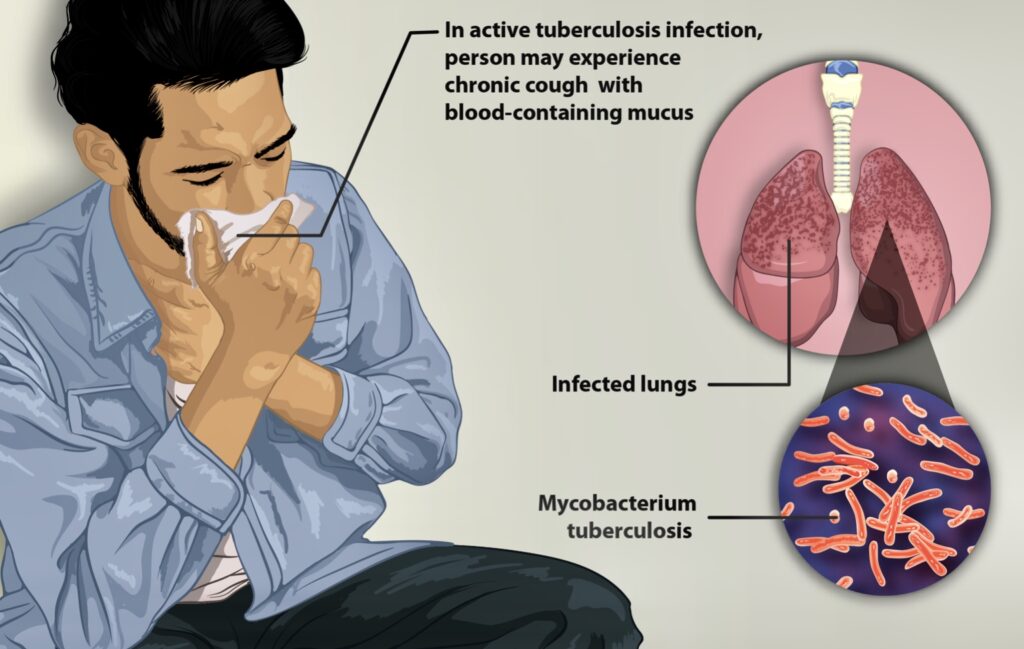
How TB attacks (Wikipedia) 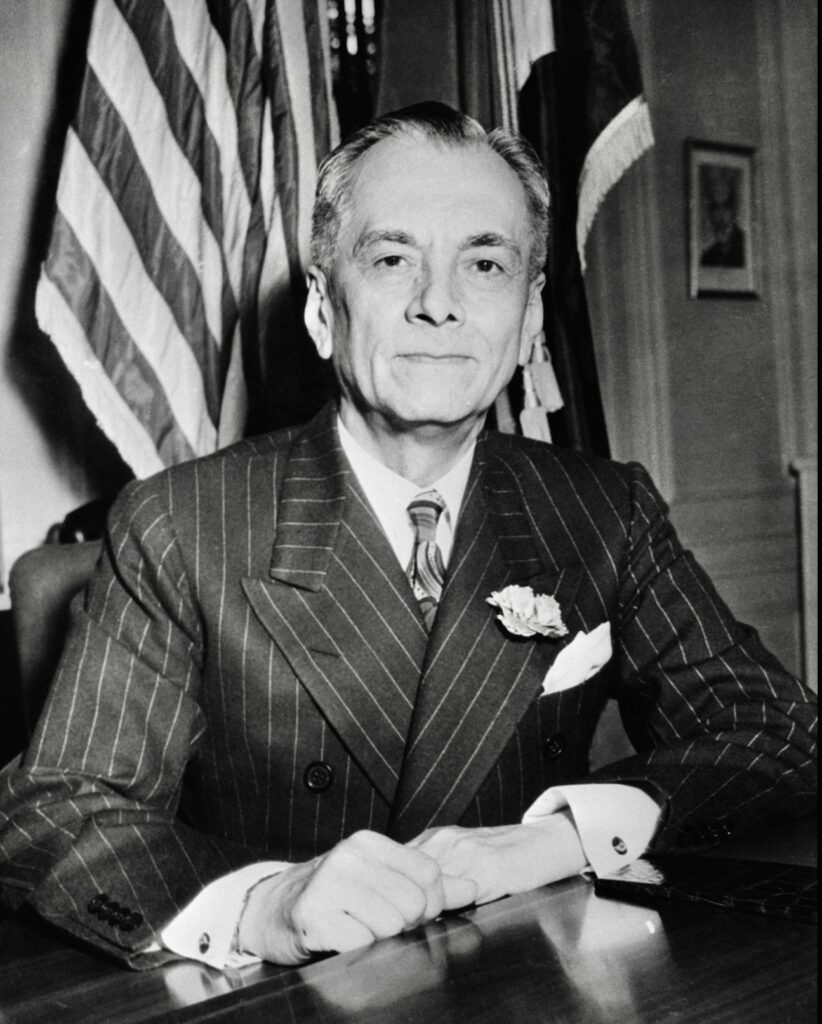
Manuel Quezon died of TB
Dr. Duque said that, unlike other health programs, having fewer cases is not an indicator of success for the country’s TB program. “Our goal for our TB program is to find and treat as many TB cases as possible,” he said. “Only by finding and treating these cases can we limit its spread and achieve our dream of a TB-free Philippines.”
Despite advanced knowledge in science and the recent discovery of sophisticated drug regimes, the disease has continued its deadly progression. “Tuberculosis is perhaps the greatest killer of all time,” wrote Dr. Frank Ryan, author of Tuberculosis: The Greatest Story Never Told. “Tuberculosis rose slowly, silently, seeping into the homes of millions, like an ageless miasma. Once arrived, TB stayed (and become) a stealthy predator.”
The tenacious TB bacillus has preyed on people since antiquity. TB-induced skeletal deformities point to the disease’s existence as early as 8000 BC. Unmistakable signs of tubercular bone decay were found in the skeletons of Egyptian mummies as long ago as 2400 BC.
“Year after year, century after century, it tightened its relentless grip, worsening with wars and famines that reduced people’s resistance, infecting virtually everyone but inexplicably sparing some while destroying others,” wrote Dr. Frank in his book.
Dr. Willie T. Ong, who co-authored the book with his wife, Dr. Liza Ong, Doctors’ Health Tips and Home Remedies, defines TB as “an infection caused by bacteria that usually affects the lungs.” These bacteria, called Mycobacterium tuberculosis (MTB), can transfer to another person through tiny droplets spread by coughing and sneezing.
This is how TB attacks the lungs: Airborne TB bacteria (bacilli) are inhaled into the lungs’ small tubes. Macrophages, a kind of defensive cell, attack the particles, killing or surrounding them. Other immune cells surround particles in hard lumps called tubercles, making bacilli harmless.
If the body’s immune system weakens, bacilli can escape from the tubercle. A weakened immune system can’t neutralize the bacilli. They multiply and penetrate blood vessels, spreading diseases throughout the body.
TB generally affects all age groups, especially children and adults with underlying conditions such as human immunodeficiency virus (HIV), malnutrition, or diabetes. Adults who smoke tobacco also have a higher risk of contracting the disease.
Fever, dry cough, and tiredness are the three most common symptoms of COVID-19. But TB is more than those symptoms. The cough is chronic and lasts more than two weeks. The person may also experience weight loss, fever, and night sweats.
“If you ever experience these symptoms, it is best to visit the nearest health center or TB clinic right away to get checked up,” the health department urged. If you are unsure of their location, you can use the online self-assessment tool – https://assessment.tbfree.ph – to find the nearest health center or TB clinic in your area.
Actually, TB has two types of infections: active TB and latent TB.
“In the case of active TB, the individual who is carrying the organism has active symptoms and can transmit the infection to other people,” the DOH explained. “On the other hand, those who have latent TB do not exhibit any of the symptoms since their immunity is able to fight off the infection. However, at some point in their life, the bacteria can reactivate and become an active TB case.”
According to the health department, TB can directly affect different parts of your body. For instance, the most common form of TB is pulmonary tuberculosis (PTB) which primarily affects a patient’s lungs. Another is extrapulmonary tuberculosis (EPTB), a form of TB that affects other parts of your organs and body, including lymphatic, pleural, and bone or joint disease, which are the most common.
The three remaining forms of TB – pericardial, meningeal, and miliary – are “more likely to result in a fatal outcome.”
Tuberculosis pericarditis, a rare disease, is an infection of the pericardium with tubercle bacilli. On the other hand, tuberculosis meningitis is a form of meningitis characterized by inflammation of the membranes around the brain or spinal cord and caused by MTB. Meanwhile, miliary tuberculosis is characterized by wide dissemination into the human body and by the tiny size of the lesions.
In the past, TB was considered the world’s deadliest disease. Then, in 1944, 21-year-old “Patricia” with progressive, far-advanced pulmonary TB received the first injection of streptomycin. She improved dramatically during the ensuing five months and was discharged in 1947. She was evaluated in 1954 and found to be healthy and the happy mother of three children.
“This injection began the age of modern anti-TB treatment and led – until recently – to dramatic reductions in TB in industrialized countries,” the United Nations health agency pointed out.
Despite being infectious and potentially fatal, TB can be cured with proper treatment and early detection.
“The first thing people with presumptive TB need to do is schedule a chest x-ray test. If it is detected as possible TB, ask your doctor for a TB sputum diagnostic test to confirm if it is really TB,” the DOH states. “It is best advised to take the sample in the morning right before eating. Patients must then gargle water and take their sputum samples outdoors or in an open and airy place away from other people.”
If results come back positive, the patient must return to their doctor to begin treatment. TB medicine is free at the nearest health center or TB clinic in your area.
“There are no ifs and buts,” Dr. Ong says. “It’s for your own good and for the good of the people around you. If you don’t take the medications, then you will be infecting an average of 10 persons in a year, including your loved ones and children.”
According to Dr. Ong, the treatment for TB is a bit more complicated compared to ordinary infections “since it will take approximately 6 months to completely eradicate the bacteria.” In cases where the infection is serious, it may take about nine months of treatment.
Only a doctor can give you the correct treatment, so you better see one. “Never self-medicate,” Dr. Ong urges. “This is the worst thing you can do. It will only strengthen the bacteria inside you and make you resistant in one tablet.”
For the six-month treatment, 3 to 4 drugs are required, usually Isoniazid, Rifampicin, Ethambutol, and Pyrazinamide. There are some preparations that have 3 or 4 drugs combined in one tablet.
“The usual TB treatment regimen is to take the four drug combinations (such as Myrin P forte) for 2 months, then followed by 2 or 3 drug combinations (such as Myrin P) for 4 months,” Dr. Ong informs.
Approximately 3-5 tablets of the medicines are taken every day – depending on the person’s body weight.
Dr. Ong suggests that those who are undergoing treatment stay at home during the first three weeks of treatment. “Don’t go to school, work or come in close contact with people,” he says. “Your saliva and phlegm can infect others.”
He also recommends that they wear a face mask during the first three weeks of treatment. “Cover your mouth with a tissue when you cough, sneeze or laugh too hard,” Dr. Ong urges. “Then throw the tissue away in a sealed container.”
It is recommended that all TB medications be taken one hour before meals. “It is ideal not to break the dose of the drug,” Dr. Ong reminds. The patient needs to see his doctor to undergo blood tests to check for possible liver side effects of the drugs taken.
Side effects aren’t common, but some TB medicines can occasionally be harmful to the liver, he says. In addition, the color of the urine will change from yellow to orange. But don’t worry; the change of color is “a normal reaction to the treatment course.”
Dr. Ong suggests that you need to consult your doctor once you experience any of the following: nausea, vomiting, loss of appetites, yellowing of the skin, or fever of more than three days.
The most important thing: “Complete the 6 to 9-month course of your medicines,” Dr. Ong declares. “Do not stop your medicines without your doctor’s permission.”
Doing so will cause the TB bacteria to be resistant to the TB drugs and may become a drug-resistant TB. If a person is classified under multidrug-resistant TB (MDR-TB), then the TB bacteria are resistant to at least isoniazid and rifampin, the two most potent TB drugs. Patients who fall under MDR-TB undergo a different type of treatment.
Meanwhile, to help solve this public health issue, the United States Agency for International Development (USAID) launched the USAID TB Innovations Project in partnership with the health department. Through this project, the #TBFreePH campaign was initiated.
#TBFreePH is the national strategy to achieve a TB-free Philippines by the year 2035. It is aligned with the Philippine (PhilSTEP) vision of a TB-free Philippines. Through a collaborative, cohesive, and comprehensive communication approach, the strategy envisions heightened attention to TB, promotes people-centered care, and reduces stigma. The mission is to elevate discourse about TB and get many more stakeholders to talk about TB.

