By Henrylito D. Tacio

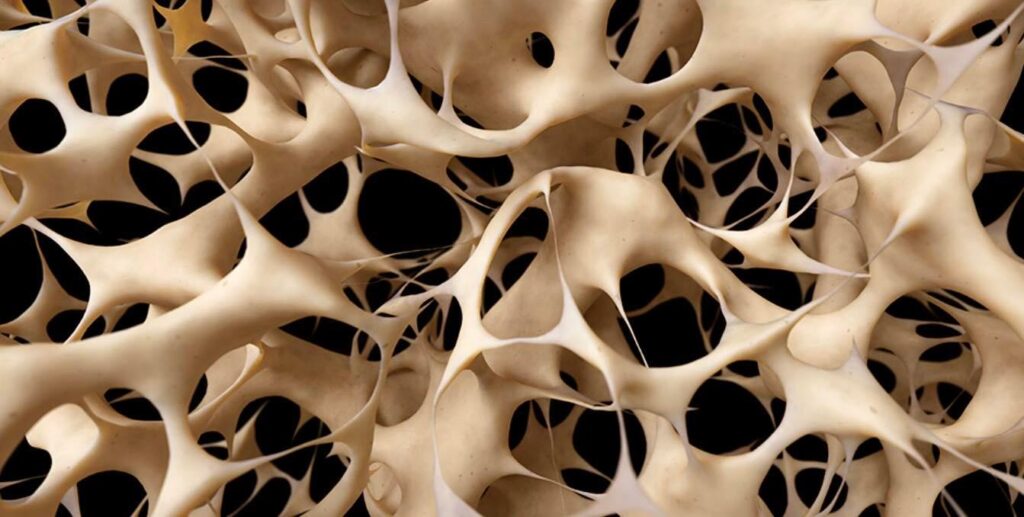
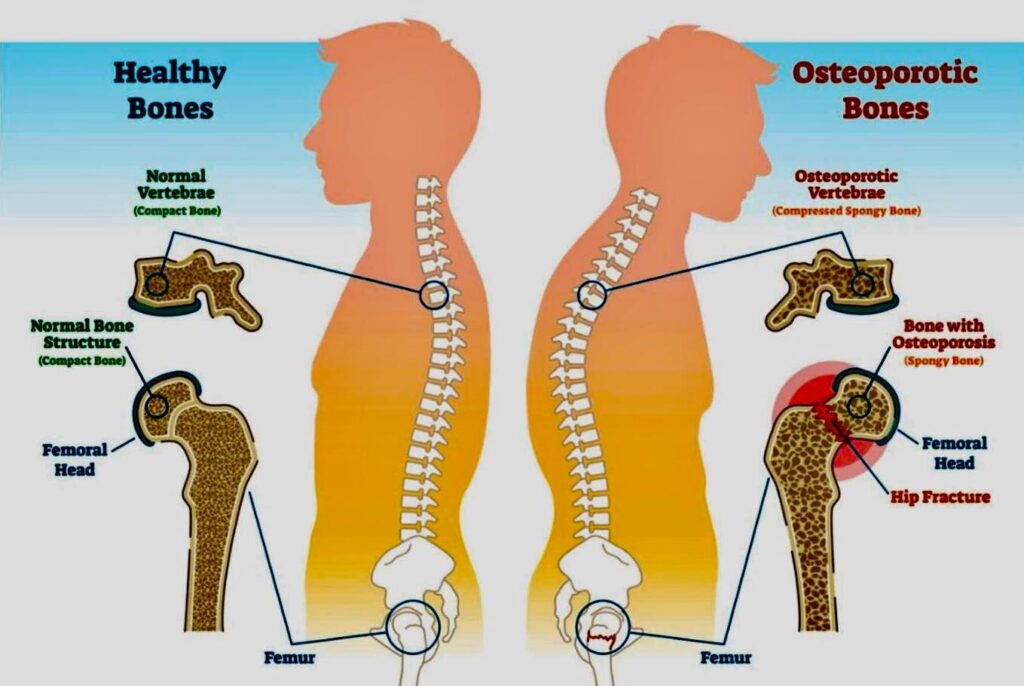
Osteoporosis comes from the two Greek words, ostoun meaning “bone” and poros which means “pore.” Literally, osteoporosis means “brittle” or “porous bones.” Actually, it is a disease that is characterized by low bone mass, deterioration of bone tissue, and disruption of bone microarchitecture. If not treated, it can lead to compromised bone strength and an increase in the risk of fracture.
“Osteoporosis is a risk factor for fracture just as hypertension is for stroke,” said a study published in the European Journal of Rheumatology. “Osteoporosis affects an enormous number of people, of both sexes and all races, and its prevalence will increase as the population ages.”
In the Philippines, the number of the elderly was 2.8 million in 2013. The figure is expected to grow to 13.4 million by 2050. “From these numbers, it has been projected that the number of Filipinos at high risk for osteoporosis will reach 10.2 million by 2050,” says the IOF-Philippines.
Osteoporosis is very different from osteoarthritis, where there is pain in a joint, like the knee or hip. “With osteoporosis, you cannot feel your bones getting weaker and pain occurs only when a bone has already been broken,” explains Dr. Monica Therese Cating-Cabral, an internist and endocrinologist, with a special interest in bone health and mineral disorders.
The weakening of bones can be taking place very quietly for years, even decades. This is the reason why it is called a “silent disease.” As Dr. Eric Jason Amante, a specialist in internal medicine, particularly in rheumatology at Manila Doctors Hospital, told ABS-CBN’s Salamat Dok, “Until our bone breaks, we don’t know we have the condition.”
As such, Dr. Cating-Cabral considered osteoporosis a serious disease. “Breaking a bone can cause permanent pain and immobility,” she wrote. “Patients may become shorter and have a hunched posture. If immobility causes them to lose their independence results in the need for long-term care, depression may set in.
“Having one fracture greatly increases the probability of another fracture within the next year,” she continued. “For elderly patients who break a hip, there is also an increased chance of dying from complications related to the fracture.”
Unfortunately, most Filipinos don’t consider osteoporosis a serious disease. “Osteoporosis is largely seen as a natural process of aging so the overall level of urgency and concern about the disease is not high,” IOF deplores.
So much so the government does not include osteoporosis in its national health priority programs. “Since the government focuses more on communicable diseases, funds are prioritized on these conditions,” IOF says.
Awareness about this bone disorder is still very low among Filipinos. A study conducted in 1995 showed that among Asians, Filipinos have the lowest awareness about this disease.
Most Filipinos, for instance, don’t know that osteoporosis is most common among women. Statistics showed that osteoporosis is four times more common in women than in men. There are several reasons for this, according to the US National Osteoporosis Foundation (NOF).
“Women tend to have smaller, thinner bones than men,” the NOF explains. “Estrogen, a hormone in women that protect bones, decreases sharply when women reach menopause, which can cause bone loss.”
On why men are lower risk of osteoporosis, the website of the health department of Australia says men generally have a larger skeleton and they don’t experience the sudden drop in hormone levels. “The decrease in bone mass occurs at a slower rate in men than women until the age of 65-70, when the rate is the same for men and women,” it stresses.
Age also plays a big part. In a study which appeared in Philippine Journal of Internal Medicine, it was reported that the overall prevalence of osteoporosis in adult Filipinos 60 to 69 years of age was 0.8% while those beyond 70 years old was 2.5%.
The National Nutrition and Health Survey states that almost 80% of Filipino women and 60% of men aged over 70, are at high risk of developing osteoporosis. This data was in 2003 yet.
Aside from gender and age, osteoporosis is also common among people who have too much or too little of certain hormones in their bodies. It is more likely to occur in people who have low calcium intake (particularly those who don’t drink milk), eating disorders (thus severely restricting food intake and becoming underweight), and gastrointestinal surgery.
The following medical conditions can also trigger osteoporosis: celiac disease, kidney or liver disease, inflammatory bowel disease, cancer, lupus, multiple myeloma, and rheumatoid arthritis.
Because official diagnosis of osteoporosis often comes too late – after a fracture – the strategy is to start fighting bone less early and to never let up. As Dr. Manju Chandran, Director of the Osteoporosis and Bone Metabolism Unit (Department of Endocrinology) at the Singapore General Hospital puts it: “Even if you already reach our peak bone mass, you should still aim to reduce bone loss and encourage new bone growth. It is only when bone loss is greater than new bone growth that osteoporosis sets in.”
To think of, you have many weapons in your arsenal, according to The Doctors Book of Home Remedies. Here are some:
1. Get enough calcium and Vitamin D
Calcium is required to support bone growth, bone healing, and maintain bone strength and is one aspect of treatment for osteoporosis. Those who are 65 and older should eat at least 700mg of calcium a day. Good sources of calcium include milk, cheese, certain vegetable greens and calcium-fortified food such as juices, cereals and breads.
Several studies have shown that a high intake of vitamin D reduces fractures in the elderly. Apart from getting vitamin D from our food, another good source is sunlight.
2. Eat a balanced diet
Eating a balanced diet ensures you get enough phosphorus and other minerals, like magnesium, vitamin K, vitamin B6 and vitamin B12 that are also essential for healthy bones.
Everydiet.org recommends: “The best source of all the nutrients you need is in a sensible balanced diet with plenty of fruit, vegetables, beans, yogurt, bread and potatoes, plus smaller amounts of very lean meat, low-fat cheese and oily fish (especially sardines), plus at least 250 ml of low-fat milk per day.”
3. Limit your alcohol intake
WebMD.com gives this information: “Regular consumption of 2 to 3 ounces of alcohol every day increases the risk of osteoporosis. It interferes with the absorption and use of calcium and vitamin D and other bone nutrients.”
“Drink only in moderation – no more than one or two drinks per day for men, and more than one drink per day for women,” suggests Dr. Cooper.
4. Moderate your intake of caffeine
Caffeine, found in coffee and tea, appears to decrease calcium absorption by a small amount. Drinking more than three cups of coffee every day may be harmful to bone health. If you enjoy drinking coffee and tea, you can help to make up for any calcium loss by getting enough calcium to meet your body’s needs. Also keep in mind that caffeine is often added to soft drinks.
5. Cut down on salty food
Eating foods that have a lot of salt causes your body to lose calcium and can lead to bone loss. “The more sodium in your diet, the more sodium you excrete – and the more sodium you excrete, the more calcium you excrete,” explains Dr. Morris Notelovitz, author of Stand Tall! The Informed Woman’s Guide to Preventing Osteoporosis. “What probably happens is that as calcium is being excreted in the urine, the blood levels of calcium drop, causing the release of parathyroid hormone, which breaks down bone to restore calcium levels.”
6. Don’t smoke
Smoking is thought to increase bone loss by reducing the absorption of calcium in the body.
Smoking one pack of cigarettes per day throughout adult life can itself lead to loss of 5-10 percent of bone mass,” says Dr. William C. Shiel. Jr., a fellow of the American Colleges of Physicians and Rheumatology. “Smoking cigarettes decreases estrogen levels and can lead to bone loss in women before menopause. Smoking cigarettes also can lead to earlier menopause. In postmenopausal women, smoking is linked with increased risk of osteoporosis.”
7. Exercise to build bones
“If you don’t exercise, you lose bone,” says Dr. Robert Heaney, a professor at the Creighton University in Omaha, Nebraska. Exercise makes bones stronger and denser.
But there are even more reasons to exercise. The benefit of exercise for osteoporosis has mostly to do with decreasing the risk of falls, probably because balance is improved and/or muscle strength is increased. Research has not yet determined what type of exercise is best for osteoporosis or for how long. Until research has answered these questions, most doctors recommend weight-bearing exercise, such as walking, preferably daily.
8. Maintain a healthy weight
A low body weight increases risk of osteoporosis, as does a previous history of anorexia nervosa. But it does not mean that heavier people don’t get osteoporosis. Having a normal weight is beneficial for general health and reduces risk of other chronic conditions such as heart diseases and diabetes.
9. Monitor your medications
Some drugs can hasten bone loss, says Dr. B. Lawrence Riggs, a professor of medical research at the Mayo Clinic. Those most likely to cause problems: corticosteroids, rheumatic disorders, allergic conditions and respiratory disease; L-thyroxine, a thyroid medication; and furosemide, a diuretic often used against fluid retention associated with high blood pressure and kidney problems.
“Talk with your doctor about this possible side effect,” Dr. Riggs suggests. “If you have other risk factors as well, your doctor may want to check your bone density and, if it’s low, alter the dosage or stop the drug entirely.” – ###
Credits: bonehealthandosteoporosis.org, m-rehab.om, and endocrineweb.com