Text and Photos by Henrylito D. Tacio
Infographics by WHO
“Diabetes, long considered a disease of minor significance to world health, is now taking its place as one of the main threats to human health in the 21st century,” deplored Prof. Paul Zimmet, director of the International Diabetes Institute. “The past three decades have seen an explosive increase in the number of people with diabetes worldwide.”
While the diabetic statistics in the Philippines are relatively low compared to industrialized countries, the drastic increase is still alarming. While the country is considered a hotspot for its fast-vanishing biological diversity, it is becoming another hotspot for diabetes cases.
That’s because the prevalence rate of diabetes among Filipinos is fast growing. Currently, an estimated 8.2 million people are having diabetes (with 4 million diagnosed cases and another 4.2 million that are undiagnosed). About 500 Filipinos are added to the demographic daily.
“It is alarming because of the fact that we may not be in the Top 10, but we are in the Top 15. We are poised to be in the Top 10 if we don’t change the way our diabetes is increasing here in the Philippines,” Dr. Ma. Cecille Anonuevo-Cruz, a fellow with the Philippine Society of Endocrinology, Diabetes, and Metabolism (PSEDM), was quoted as saying a few years back.
Diabetes, as defined by the Merck Manual of Medical Information, is “a disorder in which blood sugar (glucose) levels are abnormally high because the body does not produce enough insulin.”
Before probing deeper, let’s discuss first this hormone released from the pancreas called insulin. “Insulin controls the amount of sugar in the blood,” explains the Merck manual. “When a person eats or drinks, food is broken down into materials, including sugar, that the body needs to function.
“Sugar is absorbed into the bloodstream and stimulates the pancreas to produce insulin,” the manual further explains. “Insulin allows sugar to move from the blood into the cells. Once inside the cells, sugar is converted to energy, which is either used immediately or stored until it is needed.”
The levels of sugar in our blood vary normally throughout the day. “They rise after a meal and return to normal within about 2 hours after eating,” the Merck manual informs. “Once the levels of sugar in the blood return to normal, insulin production decreases.”
But with diabetes, something goes awry, health experts claim. The pancreas becomes irresponsible. It either stops producing the hormone completely or else produces too much, which leads to insulin resistance. Either way, the concentration of sugar in the blood shoots sky-high.
Of course, the body tries to eliminate the sugar. “The best to do is via the urine,” says Dr. Isadore Rosenfeld, author of The Best Treatment. “But since the kidneys can’t excrete sugar in lump form, the body must provide enough water to dilute or dissolve the sugar in order to flush it out.”
The net result of all this is that the person will spend more and more time in the bathroom to void the sugar and at the water tap to drink the much-needed extra water. This is the basis why the cardinal signs of untreated diabetes are frequent urination and great thirst. In women, the urine rich in sugar provides a good medium for fungus to grow in the vagina, hence the vaginal itching.
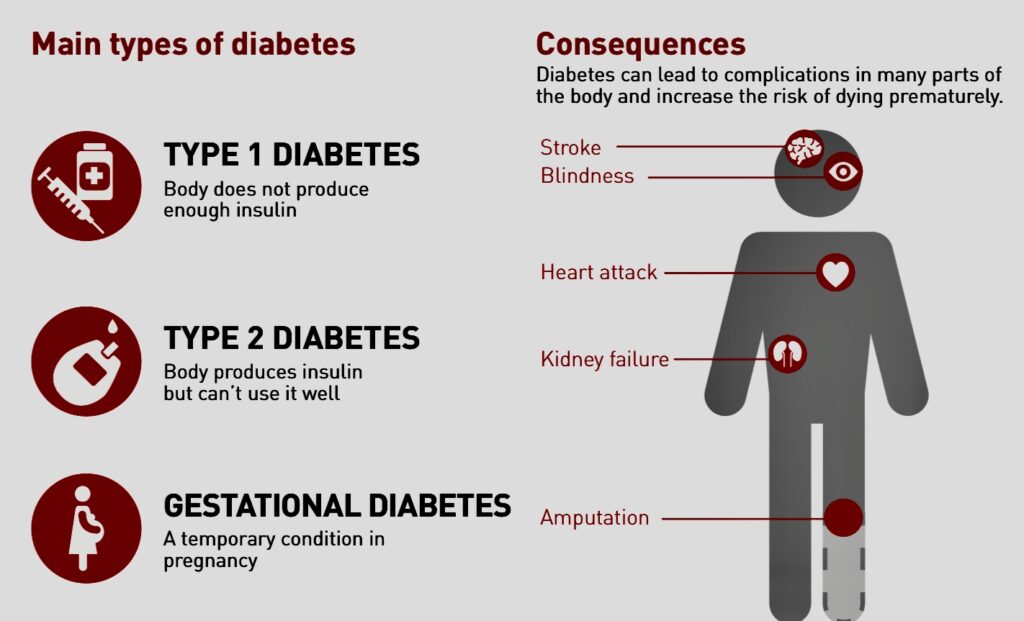
Actually, there are two forms of diabetes. Type 1 diabetes (also known as insulin-dependent diabetes) is caused by a reduction in the level of insulin. The body’s immune system destroys the insulin-producing cells in the pancreas, causing insulin deficiency. As a result, individuals with this type of diabetes need regular insulin injections to maintain glucose control.
In contrast, type 2 diabetes (also called as non-insulin-dependent diabetes) arises in the first instance not because there is a lack of insulin but because the body fails to respond to circulating insulin effectively. This condition is known as insulin resistance. For this reason, newly diagnosed individuals do not require insulin injections.

Maruya 
Sugar-rich food
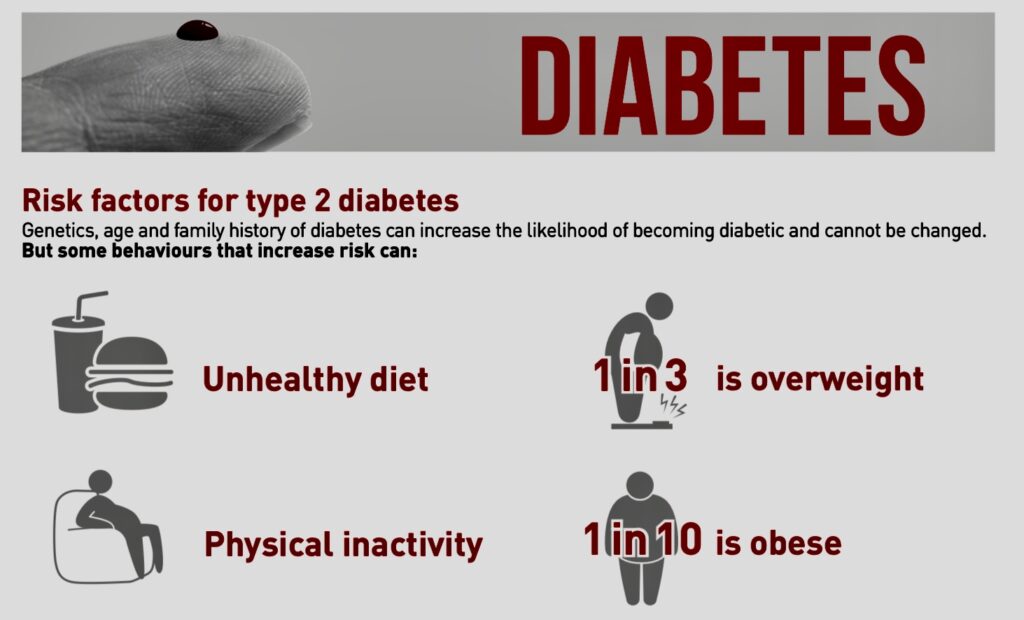
“If you look at the spread of the scourge around the world, Type 2 diabetes occurs as a country advances technologically, when people come out of the fields to sit behind desks,” notes Dr. Irwin Brodsky, director of the Diabetes Treatment Program at the University of Illinois in Chicago.
Type 2 is the strain most people have to fear. This is the real epidemic, accounting for 85-90 percent of diabetes cases in the country. “Getting diagnosed early is important because most of its serious complications are preventable,” assures Dr. Marie Yvette Rosales-Amante, who had her fellowship in endocrinology, diabetes, and metabolism at the University of Massachusetts.
Diabetes is associated with a range of complications that are largely related to damaged blood vessels and nerve cells caused by consistently high blood glucose concentrations. These complications include retinopathy (eye problems, in some cases leading to blindness), nephropathy (kidney disease), neuropathy (nerve disease which can lead to the need for amputation), heart attack, stroke, frequent infections, and impotence.
The World Health Organization (WHO) says diabetes has become one of the major causes of premature illness and death in most countries, mainly through the increased risk of cardiovascular disease.
“Because of its chronic nature, the severity of its complications and the means required to control them, diabetes is a costly disease, not only for the affected individual and his/her family, but also for the health authorities,” the United Nations health agency says.
Direct costs to individuals and their families include medical care, drugs, insulin, and other supplies. Patients may also have to bear other personal costs, such as increased payments for health, life, and automobile insurance.
Direct costs to the health care sector include hospital services, physician services, lab tests, and the daily management of diabetes (including the availability of products such as insulin, syringes, oral hypoglycemic agents, and blood-testing equipment).
“A number of diabetes may not be able to continue working or work as effectively as they could before the onset of their condition,” the WHO says. “Sickness, absence, disability, premature retirement or premature mortality can cause loss of productivity.”
The Philippine Diabetes Association (PDA), an umbrella organization of all associations involved in the care of diabetic patients, attributes the increase of diabetic incidence in the Philippines to the lifestyle and culture of Filipinos. “For one, Filipinos love to eat,” it says. “Rice is the Filipinos’ staple food.”
Some studies have shown that the starch-rich staple can potentially release high amounts of sugar into the blood when digested. A 2007 study of Chinese women in Shanghai found that middle-aged women who ate large amounts of rice and other refined carbohydrates were at increased risk for diabetes compared to their peers who ate less.
In the United States, Americans who eat white rice on a regular basis — five or more times a week — are almost 20 percent more likely to develop diabetes than those who eat it less than once a month.
For another, Filipinos are fond of holding celebrations from fiestas, birthdays, weddings, and different holidays in which food indulgence is inherent and a crucial part of the celebrations.
“Filipinos have the best fatty, risky exotic foods,” PDA surmises. To name a few: “batsoy,” “bulalo,” liver and other organ meat, “sisig,” street foods (“isaw,” pork and chicken barbecue, “adidas”), and “lechon.”
Their condiments are among the world’s best: “bagoong” and “patis.” Filipinos also have the best and sweetest native delicacies and cakes, which are mostly prepared from rice: “puto,” “palitaw,” “biko,” and “bibingka,” among many others.
With these kinds of foods, less exercise, and too much stress, it is no wonder why there will be more diabetics in the Philippines in the years to come.